Pituitary Apoplexy
Pituitary apoplexy denotes the presence of hemorrhagic necrosis of the pituitary, which generally occurs within a pituitary macroadenoma. In some cases, hemorrhage may occur within a cystic lesion (including Rathke’s cleft cyst). Rarely, pituitary apoplexy may occur as a result of hemorrhage within the pituitary gland in the absence of an adenoma or cyst. Pituitary apoplexy is a rare condition. In contrast, asymptomatic hemorrhage within a pituitary adenoma is not uncommon (occurring in approximately 15% of patients with pituitary adenomas).
Patients with
pituitary apoplexy present with severe headache of acute onset, which is
typically considered as the worst headache ever experienced. Nausea and
vomiting are very common. The rapid expansion of intrasellar contents
frequently leads to compression of the optic chiasm, causing visual field
defects. Lateral expansion resulting in compression of the nerves coursing
through the cavernous sinuses (including the third, fourth, fifth, and sixth
cranial nerves), fre- quently leads to diplopia, ptosis, facial pain, or
numbness. Increased intracranial pressure may occur, leading to impairment
in the level of consciousness. Interference with hypothalamic function may lead
to manifestations of sympathetic nervous system dysfunction, including
arrhythmias or disordered breathing.
In addition,
some of the blood may enter the subarachnoid space, leading to meningeal
irritation. Fever and neck stiffness may thus occur. Analysis of the
cerebrospinal fluid may reveal the presence of red cells and increased protein
content. It is therefore apparent that pituitary apoplexy should be considered
in the differential diagnosis of patients with suspected subarachnoid
hemorrhage or meningitis.
Life-threatening
pituitary failure may occur as a result of central hypoadrenalism (adrenal crisis).
Anterior hypopituitarism has been reported in up to 90% of patients with
pituitary apoplexy. In contrast, central diabetes insipidus is uncommon.
Pituitary
apoplexy is often spontaneous and often occurs at presentation of a pituitary
adenoma. Identified risk factors for the development of pituitary apoplexy
include trauma, anticoagulant use (including heparin or warfarin), coagulation
disorders, and administration of dopamine agonists (including bromocriptine or
cabergoline) or hypothalamic-releasing hormones.
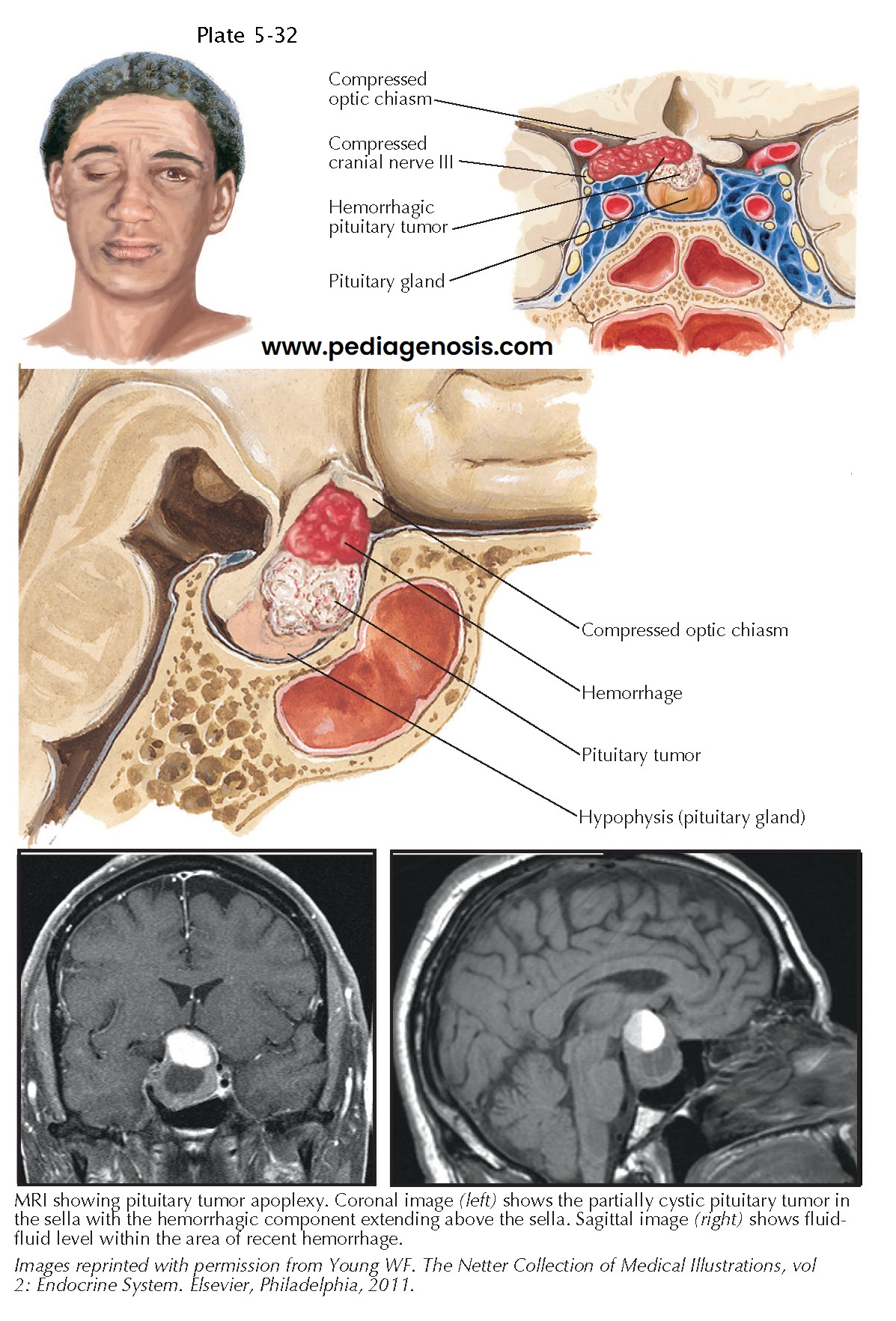
Magnetic
resonance imaging typically reveals a focus of hyperintensity (on noncontrast
T1-weighted images) within a sellar mass. A fluid-fluid level may also be
evident. Impingement on the optic chiasm or the cavernous sinuses is frequently
present. Laboratory testing usually reveals evidence of hypopituitarism.
Pituitary
apoplexy is a medical and neurosurgical emergency. These patients should be
hospitalized and receive at minimum a stress dose glucocorticoid coverage to
prevent the development of adrenal crisis. Of note, pharmacologic doses of
glucocorticoids are often administered to minimize acute pressure effects from
the hemorrhagic sellar mass on neighboring structures. Patients with impaired
level of consciousness or other evidence of increased intracranial pressure,
visual field defects, diplopia, or ptosis should be considered for early
(within 1 week) neurosurgical decompression, generally performed via the
trans-sphenoidal route. Early pituitary surgery is associated with more complete
recovery of visual field deficits than observation.
In contrast, patients who maintain a normal level of consciousness and show no evidence of increased intracranial pressure, visual field defects, or ophthalmoplegia may be observed. These patients may be considered for pituitary surgery if the sellar mass fails to regress considerably after the hemorrhage is reabsorbed. Pituitary function needs to be monitored and hormone replacement therapies advised as required. Hypopituitarism is often per anent, regardless of whether surgery is performed.