PELLAGRA
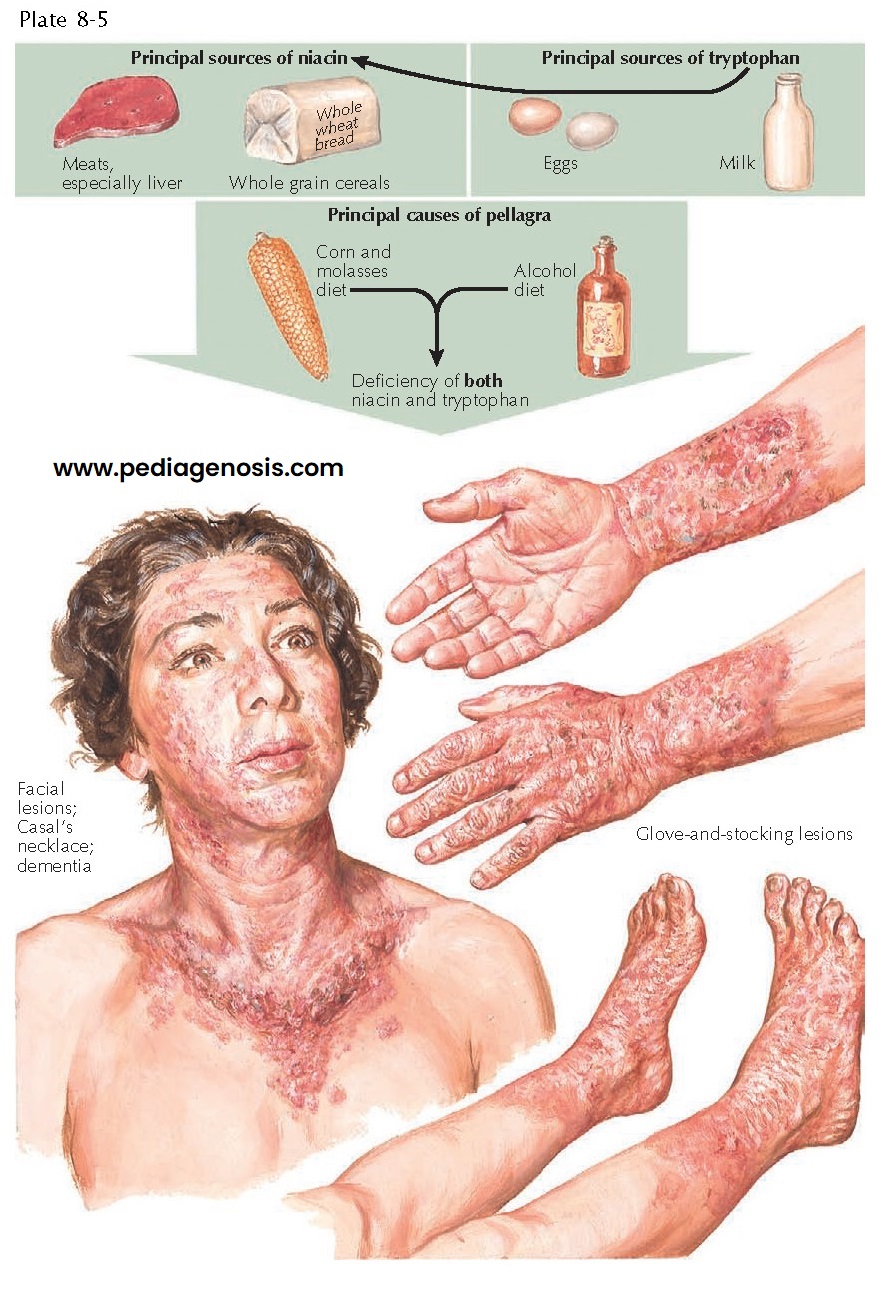 |
| MAIN SOURCES, CAUSES, AND SKIN FINDINGS OF PELLAGRA |
Pellagra is caused by inadequate dietary intake of niacin (nicotinic acid, vitamin B3) or its precursor amino acid, tryptophan. It has also been discovered to occur on occasion in patients with carcinoid syndrome. In this syndrome, tryptophan is used entirely to produce serotonin, and there is none left to produce niacin. Pellagra was first identified as a unique disease in the early 1700s by a Spanish physician, Gaspar Casal, who observed it in Spanish peasants who ate diets almost entirely made of corn and corn-based foodstuffs. He named the disease “Asturian leprosy” after the region of Spain he was studying. An Italian physician, Francesco Frapoli, who studied the disease in endemic regions of northern Italy, later named it pellagra.
Pellagra
has been dominant in regions of the world that rely heavily on corn as the main
dietary staple. In the early twentieth century, the southern United States was
inundated with cases of pellagra. Joseph Gold-berger, a physician and
epidemiologist studying the disease, discovered that pellagra was caused
directly by a deficiency of vitamin B. He was unable at that time to isolate
the specific B vitamin, but he has been given credit for discovering the cause
of pellagra.
Clinical Findings: Pellagra can affect any individual
regardless of race or gender. The incidence in the North America and Europe is
low, and cases are mainly caused by abnormal diets and alcoholism. The disease
can still be seen in endemic regions of the world where corn is the main food
source. The clinical cutaneous hallmark of pellagra is a severe dermatitis. The
dermatitis is photosensitive, and exposure to the sun often brings out the rash
or exacerbates it. Patients often present initially after having spent many hours
outdoors on an early spring day. The dermatitis is symmetric and is manifested
by eczematous patches and thin plaques that tend to be tender to the touch.
There is a fine line of demarcation between abnormal and normal skin. The head,
neck, and arms are the most involved regions because of their higher level of
sun exposure. The dermatitis along the anterior neck and upper thorax has been
termed Casal necklace. This is represented by weeping pink and red patches and
plaques in a distribution like that of a necklace touching the skin
circumferentially around the neck. Because of its photosensitive nature, the
dermatitis of pellagra often spares the skin directly behind the ears and
beneath the chin. The nose, forehead,
and cheeks are prime regions of involvement. Non–sun-exposed areas can also be
involved, and the intertriginous regions are almost universally affected,
including the perineum, axillae, and inframammary skin folds. The reason for
the propensity to affect these non–sun-exposed regions is poorly understood but
may be related to chronic friction that induces the dermatitis. In the areas of
involvement, small vesiculations may occur because of separation of the
epidermis from the dermis.
As
time progresses, the dermatitis begins to desquamate. This process begins in
the central portions of the dermatitis and spreads outward in a centrifugal
manner. As the skin desquamates, it leaves behind red, eroded patches and
plaques. Chronic involvement leaves permanent scarring and abnormal
hyperpigmentation or hypopigmentation of the area. The epidermis over bony
prominences (e.g., ulnar head) shows marked hyperkeratosis.
Mucous
membrane involvement is common in all vitamin deficiency states, and pellagra
is no exception. Angular cheilitis and a red, shiny, edematous tongue with
atrophied papillae are seen routinely in patients with pellagra. The oral and
gastrointestinal mucous membranes may be involved. Oral ulcerations are
frequently seen. Patients routinely complain of a sore mouth and difficulty
swallowing; these symptoms can lead to further lack of proper nutrition,
exacerbating and compounding the disease.
Diarrhea
is commonplace and is caused by the effect of niacin deficiency on the
gastrointestinal tract. The diarrhea is watery and further complicates the
patient’s nutritional status and electrolyte and fluid balances. Blood and
purulence may be present in the watery diarrhea as a result of ulceration and
abscess formation. Ulcerations can be seen throughout the gastrointestinal tract, as can
cystic dilation of the mucous glands. The colon may show small submucosal
abscesses.
Subtle
neurological findings precede full-blown encephalopathy in pellagra. These
clinical findings include poor concentration, headaches, and apathy. Dementia
eventually sets in as the disease causes a diffuse encephalopathy. The
encephalopathy may mimic psychiatric disease, especially depression with
suicidal tendency. Other well-defined symptoms include confusion,
hallucination, delirium, insomnia, tremor, seizures, and extrapyramidal
rigidity. The entire central nervous system is involved in severe pellagra.
Cortical nerve cells show degeneration. The Betz cells show chromatolytic
changes with displacement of the nucleus toward the cell wall. There is an
increased amount of adipose in the nerve cells as well as an increase in the
lipofuscin pigment within the cytoplasm of these cortical cells. The posterior
columns may undergo demyelination, leading to tremor, gait disturbance, and
movement difficulties. Chromatolysis has been shown to occur in the pontine
nuclei, spinal cord nuclei, and multiple cranial nerve nuclei. As the
encephalopathy progresses, disorientation and delirium take over, and the
patient eventually slips into a coma. Death may shortly ensue unless the
disease is diagnosed and treated appropriately. These unique clinical findings
seen in pellagra can be simplified in the oft-quoted mnemonic, “4 D’s”:
dermatitis, diarrhea, dementia, and death.
The
diagnosis is typically made on clinical grounds, and laboratory analysis is
used for confirmation. One should always consider other vitamin deficiencies
when evaluating a patient with pellagra. The 24-hour urine secretion of N-methyl
nicotinamide is normally in the range of 5 to 15 mg/day; in patients with
pellagra, it is less than 1.5 mg/day. Measurement of this metabolite serves as
an easy, noninvasive test to confirm the deficiency of niacin. Serum niacin
levels can be measured directly, although they are not as accurate as the
urinary excretion levels.
Histology: The skin biopsy findings are nonspecific and show
epidermal pallor with a mixed inflammatory infiltrate that is predominantly
composed of lymphocytes in a perivascular location. Occasional areas of
inflammatory vesiculation within the epidermis may be seen.
Pathogenesis: Niacin is an essential vitamin that is found in many
food sources, including whole grain breads and meats. Patients whose diet is
deficient in niacin are seen in regions of the world where corn is the main
food source. Various levels of niacin deficiency occur. This disease can also
be seen in alcoholics who do not maintain a balanced diet and receive almost
all their caloric intake from alcoholic products. Patients who develop pellagra
also have a diet deficient in tryptophan. Major sources of tryptophan include
eggs and milk. Tryptophan is a precursor of niacin and can be converted to
niacin. Niacin is required for the proper production of nicotinamide adenine
dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP),
important coenzymes for many biochemical reactions. Both molecules are
capable of acquiring two electrons and acting as reducing agents in various
reduction-oxidation (redox) reactions. When a deficiency of niacin occurs, many
biochemical reactions throughout the human body cannot be properly performed,
and the clinical manifestations occur.
Carcinoid
syndrome is a rare cause of pellagra. Carcinoid is a syndrome of excessive
secretion of serotonin.
Tryptophan
is the precursor for serotonin as well as niacin, and in this syndrome all
tryptophan is shunted to make serotonin at the expense of tryptophan. This
results in decreased production of niacin and, potentially, the clinical
symptoms of pellagra.
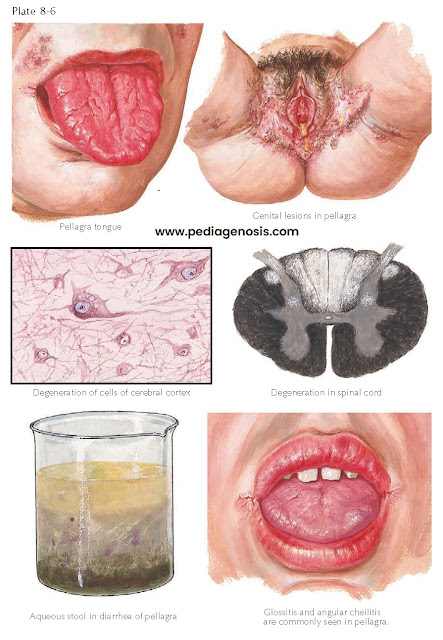 |
| MUCOSAL AND CENTRAL NERVOUS SYSTEM MANIFESTATIONS OF PELLAGRA |
Treatment: Pellagra rapidly responds to supplementation with niacin. Niacin is given orally every 6 hours until the patient responds. If a patient does not respond, a coexisting vitamin deficiency should be sought. If possible, a nutritionist should be consulted to advise the patient on proper dietary intake. Alcoholics, who can be deficient in many B vitamins, are often treated with multiple B vitamins. Patients with carcinoid syndrome need to take supplemental niacin to avoid pellagra symptoms, but the goal of therapy is to treat the underlying tumor.




