MECHANICAL VENTILATION
INDICATIONS
AND GOALS OF THERAPY
Mechanical ventilation is used when patients cannot maintain adequate gas exchange because of neuromuscular impairment, cardiovascular failure, diffuse lung disease, or disordered respiratory drive. The goals of mechanical ventilation are to improve arterial oxygenation, decrease energy consumption, and facilitate carbon dioxide (CO2) elimination so as to preserve adequate acid-base balance. Mechanical ventilation is continued until the condition responsible for respiratory failure improves and the patient can successfully resume adequate spontaneous respiration.
PRINCIPLES OF POSITIVE-PRESSURE MECHANICAL VENTILATION
To deliver a volume of gas into the lungs, a pressure
difference (Ptot) must be applied across the respiratory system to overcome
both the elastic recoil of the lung and chest wall (Pel) and the resistance
of the anatomic and artificial (i.e., ventilator tubing, endotracheal tube)
airways (Pres). This relationship can be approxima ed by the equation
of motion for the respiratory system:
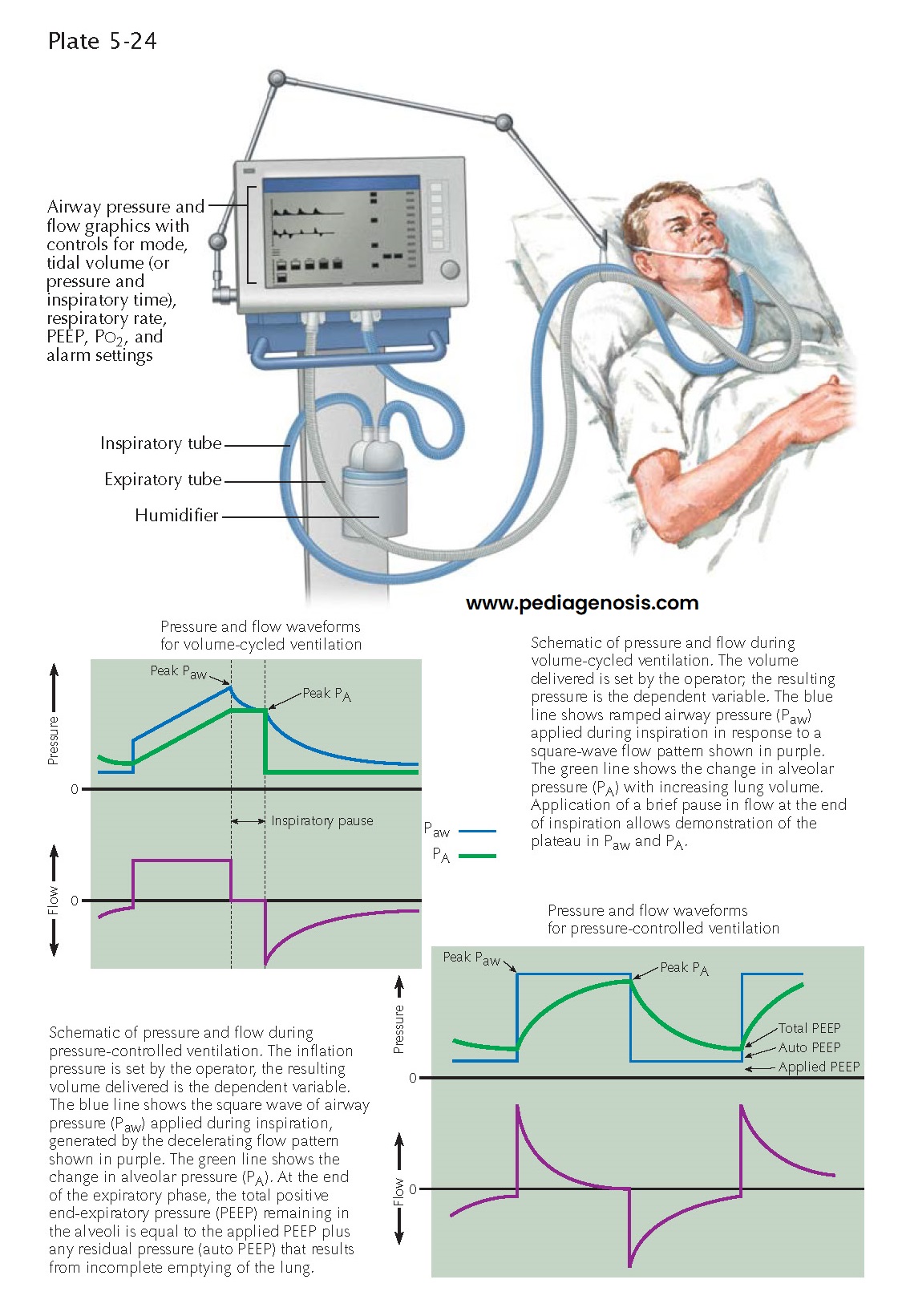
Modes of Ventilation
Mechanical ventilators must sense the patient’s respiratory efforts and then interact with these efforts with a response selected by
the clinician. Modes of ventilation refer to these different patterns of clinician-set
responses to the patient’s efforts. In full ventilatory support modes (assist/control
ventilation), a full ventilator breath is delivered either at a set time after
the last breath or in response to the patient’s respiratory efforts as detected
by changes in airway pressure or flow.
Alternatively, the clinician can set a minimum (backup) number
of machine breaths triggered by the ventilator or the patient and allow the patient
to have additional unsupported breaths above this backup rate without or with minimal
machine support, a mode called synchronized intermittent mandatory ventilation
(SIMV). Yet another option is pressure support ventilation (PSV), during
which the patient triggers each breath but the ventilator provides only enough
additional flow to maintain a clinician-set positive airway pressure. Both SIMV and
PSV can be used to gradually reduce ventilatory support. PSV is often used during
trials of spontaneous breathing to assess if mechanical ventilation can be discontinued.
Complications
After a patient has been placed on mechanical ventilation, the clinician must try to minimize the associated complications. Endotracheal and tracheotomy tubes bypass the anatomic barriers of the lung, putting patients at risk for ventilator-associated pneumonia (VAP), a serious and often fatal complication. Elevating the head of the bed 30 to 45 degrees appears to reduce aspiration and VAP incidence. Noninvasive ventilation using a tight-fitting nasal or full face mask may allow patients with chronic obstructive pulmonary disease exacerbations to avoid intubation and decrease the incidence of VAP. For patients with ARDS, use of low inspired lung volumes (6 mL/kg ideal body weight) improves outcomes by reducing additional lung injury, pneumothoraces, and hemodynamic compromise from excessive airway pressures. Because the rate of compli- cations from mechanical ventilation increase with time, it is important to evaluate patients for iberation from mechanical ventilation on a daily basis.