Innervation
of Heart
 |
| NERVES OF HEART |
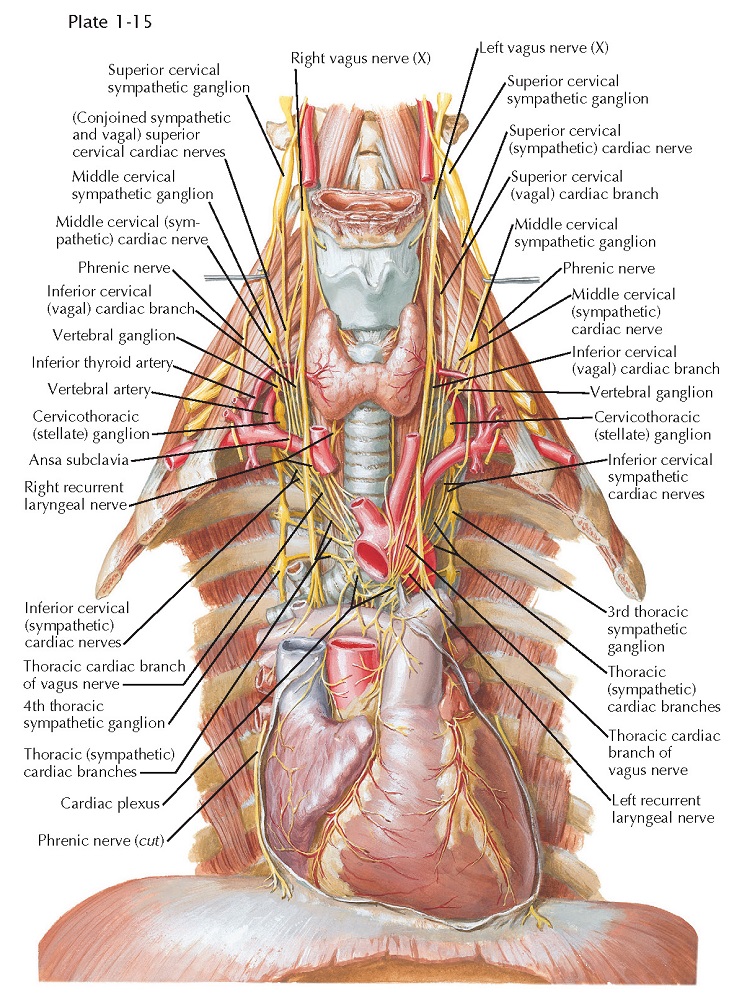
The heart is supplied by sympathetic and parasympathetic nerves that arise primarily in the cervical region because initially the heart develops in the neck. Later the heart migrates downward into the thorax, along with its nerves.
The cervical and
upper thoracic sympathetic trunk ganglia contribute cardiac branches,
all of which pass through the cardiac plexus, usually without forming
synapses. These ganglia are ultimately distributed to the various layers of the
heart wall through the coronary plexuses. Three pairs of sympathetic cardiac
nerves are derived from the cervical ganglia of the sympathetic trunks, and
others arise from the upper thoracic ganglia.
The superior cervical
sympathetic cardiac nerve originates by several rootlets from the
corresponding ganglion. It often unites with the superior vagal cardiac
nerve(s), and this conjoined nerve then descends behind the carotid
sheath, communicating en route through slender rami with the pharyngeal,
laryngeal, carotid, and thyroid nerves. On the right side, the conjoined nerve
passes posterolateral to the subclavian and brachiocephalic arteries and aortic
arch; on the left it curves downward across the left side of the aortic arch.
The middle cervical sympathetic cardiac nerve is often the largest of
the cervical cardiac nerves. It is formed by filaments from the middle and
vertebral ganglia of the sympathetic trunk. This cardiac nerve usually
runs independent of the cardiac plexus but may unite with other cardiac nerves,
and it is interconnected with tracheal, esophageal, and thyroid branches of the
sympathetic trunks.
The inferior cervical
sympathetic cardiac nerves consist of filaments arising from the stellate
(cervicothoracic) ganglion and ansa subclavia. These cardiac
nerves often combine with each other or with other cardiac nerves before
reaching the cardiac plexus, and inconstant communications exist between
these nerves and the phrenic nerves.
The thoracic
sympathetic cardiac nerves are four or five slender branches on each side
that arise from the corresponding upper thoracic sympathetic trunk ganglia.
These cardiac nerves run forward and medially to the cardiac plexus. Some enter
the plexus directly, whereas others are united for variable distances with
filaments destined for the lungs, aorta, trachea, and esophagus.
The vagal
(parasympathetic) cardiac branches vary in size, number, and arrangement but
can be grouped as superior and inferior cervical and thoracic vagal cardiac
nerves. The superior cervical vagal cardiac nerve forms from two or
three filaments that leave the vagus in the upper part of the neck and
usually unites with the corresponding sympathetic cardiac nerve. This conjoined
nerve then descends to the cardiac plexus (see earlier). The inferior
cervical vagal cardiac nerve(s), one to three in number, arise in
the lower third of the neck and often join or communicate with the cardiac
branches from the middle cervical sympathetic ganglia and the vertebral
and/or stellate sympathetic ganglia. If they remain
separate, these cardiac nerves lie posterolateral to the brachiocephalic artery
and aortic arch on the right side and lateral to the left common carotid artery
and aortic arch on the left side.
The thoracic vagal
cardiac nerves are a series of filaments arising from the vagus nerve of
each side, at or below the level of the thoracic inlet, and also from both recurrent
laryngeal nerves, with the left contributing more filaments than the right.
These often unite with other cardiac nerves in their passage to the cardiac
plexus.
CARDIAC PLEXUS
All the vagal and the
sympathetic cardiac nerves converge on the cardiac plexus, and filaments from
the right and left
sides of the plexus surround and accompany the coronary arteries and their branches.
The cardiac plexus lies between the concavity of the aortic arch and the
tracheal bifurcation and is sometimes described as consisting of superficial
and deep parts, although their depths vary minimally, and they are intimately
interconnected. However, a superficial tenuous preaortic plexus exists over the
ascending aorta.
A proportion of the vagal
fibers relay in several ganglia present in the cardiac plexus. The largest, the
ganglion of Wrisberg, lies below the aortic arch between the division of the
pulmonary trunk and the tracheal bifurcation. Other, smaller collections of parasympathetic
cells—the intrinsic cardiac ganglia—are located mainly in the atrial
subendocardial tissue, along the AV sulcus and near the roots of the great
vessels. Relatively few cardiac ganglia are found over the ventricles, but
enough exist to question the view that the ventricular innervation is entirely
or predominantly sympathetic.
The cardiac sympathetic
and parasympathetic nerves carry both afferent and efferent fibers.
The afferents transmit impulses to the central nervous system from discrete
cardiac receptor endings and terminal networks plentiful in these reflexogenous
zones, such as the endocardium around openings of the caval and pulmonary
veins, over the interatrial septum, and in the AV valves. The efferents carry
impulses that are modified reflexively by afferent impulses from the heart and
great vessels. Efferent fibers are under the overall control of the higher
centers in the brain, the hypo- thalamus, and the brainstem.
The more important
pathways are illustrated in Plates 1-15 and 1-16. Afferents from the heart and the
great vessels are shown traveling to the cord via the sympathetic cardiac
nerves, whereas others are carried upward to nuclei in the medulla
oblongata by the vagus nerves. The efferents pursue similar routes
but travel in a centrifugal direction. The cell bodies of the afferent neurons
are situated in the dorsal root ganglia of the upper four or five thoracic
nerves and in the inferior vagal ganglia.
The preganglionic
parasympathetic fibers are the axons of cells in the dorsal vagal nuclei,
and these fibers relay in cardiac plexus or intrinsic cardiac ganglia. The preganglionic
sympathetic fibers are the axons of cells located in the lateral gray
columns of the upper four or five thoracic segments. These fibers enter the
corresponding spinal nerves and leave them in white rami communicantes. which
pass to adjacent ganglia in the sympathetic trunks. Some fibers relay in these
ganglia, however, and the postganglionic fibers (the axons of ganglionic cells)
are conveyed to the heart in the thoracic sympathetic cardiac nerves.
Others ascend in the sympathetic trunks to form synapses with cells in the superior,
middle, and vertebral ganglia, and the postganglionic fibers reach
the heart via cardiac branches of these ganglia. Therefore the parasympathetic
relays occur in ganglia near or in the heart, whereas the sympathetic relays
are located in ganglia at some distance from the heart. Consequently, the
parasympathetic postganglionic fibers are relatively short and circumscribed in
their distribution.
Afferent and efferent
fibers probably run in all the sympathetic and the parasympathetic cardiac
nerves, although afferents may not be present in the superior cervical
sympathetic cardiac nerves. Many afferent vagal fibers from the heart and
great vessels are involved in reflexes depressing cardiac activity, and in some
animals these fibers are aggregated in a separate “depressor nerve” and in
humans may run in cardiac branches of the laryngeal nerves.
Despite their
insignificant size, the thoracic sympathetic cardiac nerves carry many efferent
accelerator and afferent fibers to and from the heart and great vessels. Other
cardiac pain afferents run in the middle and inferior cervical sympathetic
cardiac nerves, but after entering the corresponding cervical ganglia, they
descend within the sympathetic trunks to the thoracic region before passing
through rami communicantes into the upper four or five thoracic nerves, then to
the spinal cord.
Because many cardiac pain fibers run through the preaortic plexus, some
advocate excision of this plexus as a simpler, safer alternative to upper
thoracic sympathetic ganglionectomy for relief of angina pectoris.
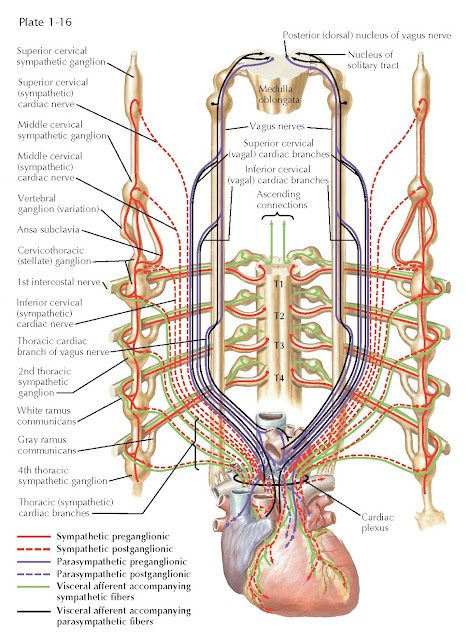 |
| SCHEMA OF INNERVATION |
Afferent fibers from the pericardium are carried mainly in the phrenic nerves, although afferents from the visceral serous pericardium are conveyed in the coronary plexuses.




