ENDOTRACHEAL SUCTION
Nasotracheal suction aids in the removal of retained bronchopulmonary secretions in patients who are unable to expectorate sputum voluntarily. However, chest physiotherapy, including postural drainage, percussion, aided coughing, and vibratory positive expiratory pressure devices, can be quite effective and are more acceptable to alert and oriented patients. The major indication for nasotracheal suction is the semicooperative or obtunded patient who requires tracheobronchial toilet.
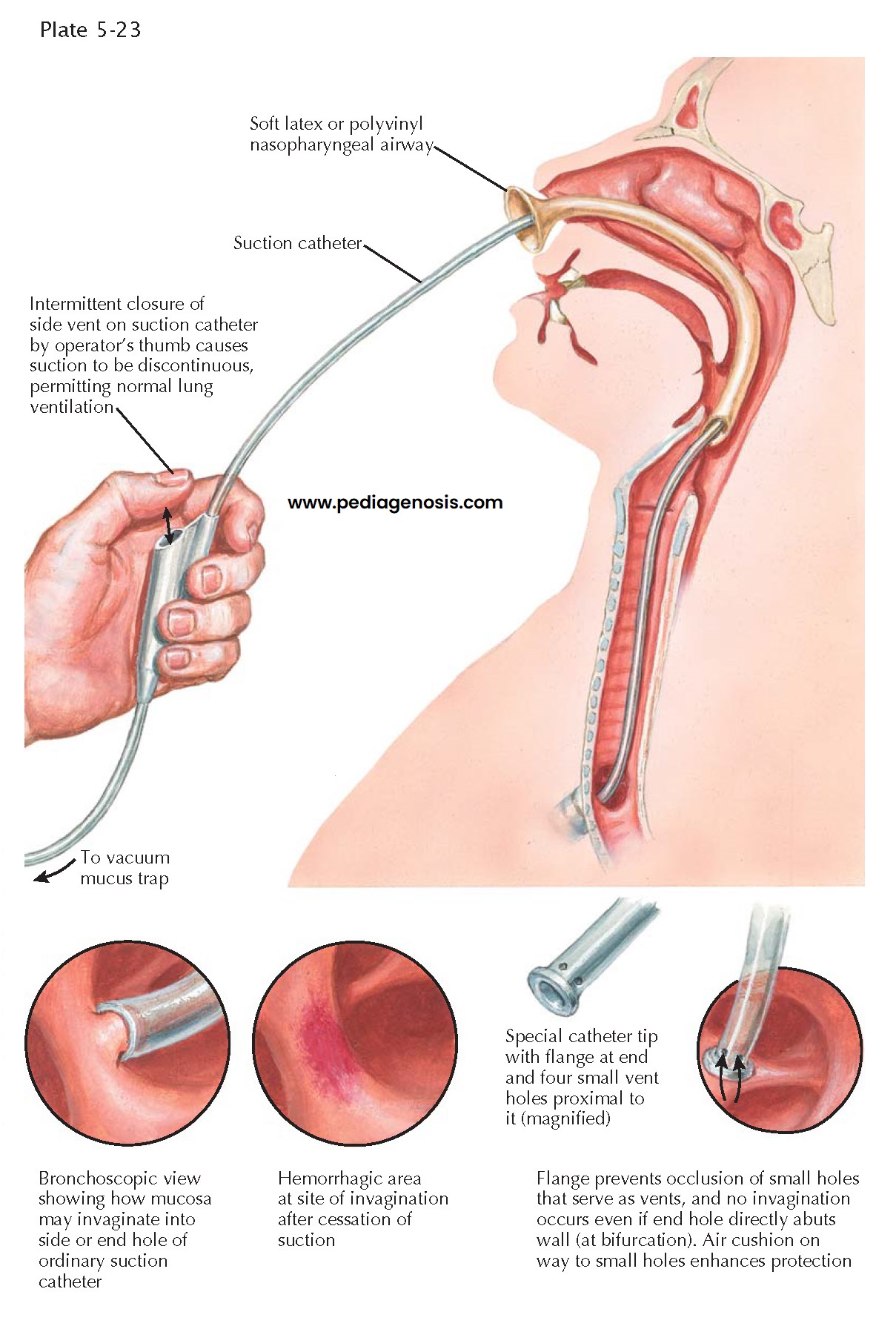
For nasotracheal suction, a soft latex or polyvinyl 32- or
34-Fr nasopharyngeal airway, lubricated with lidocaine jelly, is inserted into the
nose and advanced so that its distal tip lies above the vocal cords. A 14-Fr
suction catheter, held with a sterile-gloved hand, is then passed through the nasopharyngeal
airway and advanced with each inspiratory phase of respiration. With passage
through the vocal cords, the patient usually coughs. Introduction of the suction
catheter in this way prevents trauma to the nasal mucosa and larynx and minimizes
the deposition of upper airway secretions into the lung. Whereas approximately 90%
of attempts to reach the tracheobronchial tree by this method are successful,
the success rate for blind nasal passage ranges from 10% to 70% depending on the
operator.
After passing the vocal cords, the catheter is advanced
until it reaches the main bronchi. Because the right mainstem bronchus has a more
vertical orientation than the left mainstem bronchus, the catheter more frequently
enters the right-sided airways. The catheter is then withdrawn while the operator
intermittently makes and breaks suction (set between 100 and 160 mm Hg) over a period
of 15 to 25 seconds. The catheter is then removed and discarded after a single
pass. Nasotracheal suctioning is generally effective in removing tracheal secretions.
It also stimulates coughing, which facilitates clearance of secretions from the
major bronchi. Nasotracheal suction of left-sided secretions usually is often ineffective,
and bronchoscopic removal must be used.
Patients requiring mechanical ventilation often require “inline”
suctioning because the presence of the endotracheal tube keeps the glottis patent,
limiting the generation of sufficient intrathoracic pressure to adequately clear
secretions. By minimizing disconnections from the ventilator, inline suctioning
avoids derecruitment and reduces the risk of nosocomial infection. Hypoxemia
may be minimized by limiting the duration of suctioning to 3 to 5 seconds and administering
100% oxygen for about 1 minute before the procedure.
Suctioning through a tracheostomy tube is performed in a
similar fashion, using the inline method if the patient requires mechanical ventilation
and the “sterile” technique if the patient is receiving supplemental oxygen via
a humidified “trach collar.” Clearly, because the airway is not a sterile environment,
the procedure is not truly sterile; however, the operator should always try to minimize
nosocomial infection by wearing sterile gloves and disposing of the suction
tubing after each suctioning period.
It should be understood that all suction catheters traumatize the tracheobronchial mucosa in two ways: (1) by causing invagination of the mucosa into the end or side holes with consequent immediate ischemic necrosis of the area and (2) by direct physical contact, which results in delayed sloughing of ciliated epithelium many hours later. Erosions caused by suctioning permit colonization and penetration of the mucosa by pathogens as well as cessation of the host mechanism of mucociliary transport. Avoiding continuous suctioning and the use of a weaker vacuum tend to minimize the damage, but unfortunately, efficiency of secretion aspiration is also diminished.