COMMON NAIL DISORDERS
 |
| COMMON FINGERNAIL DISORDERS |
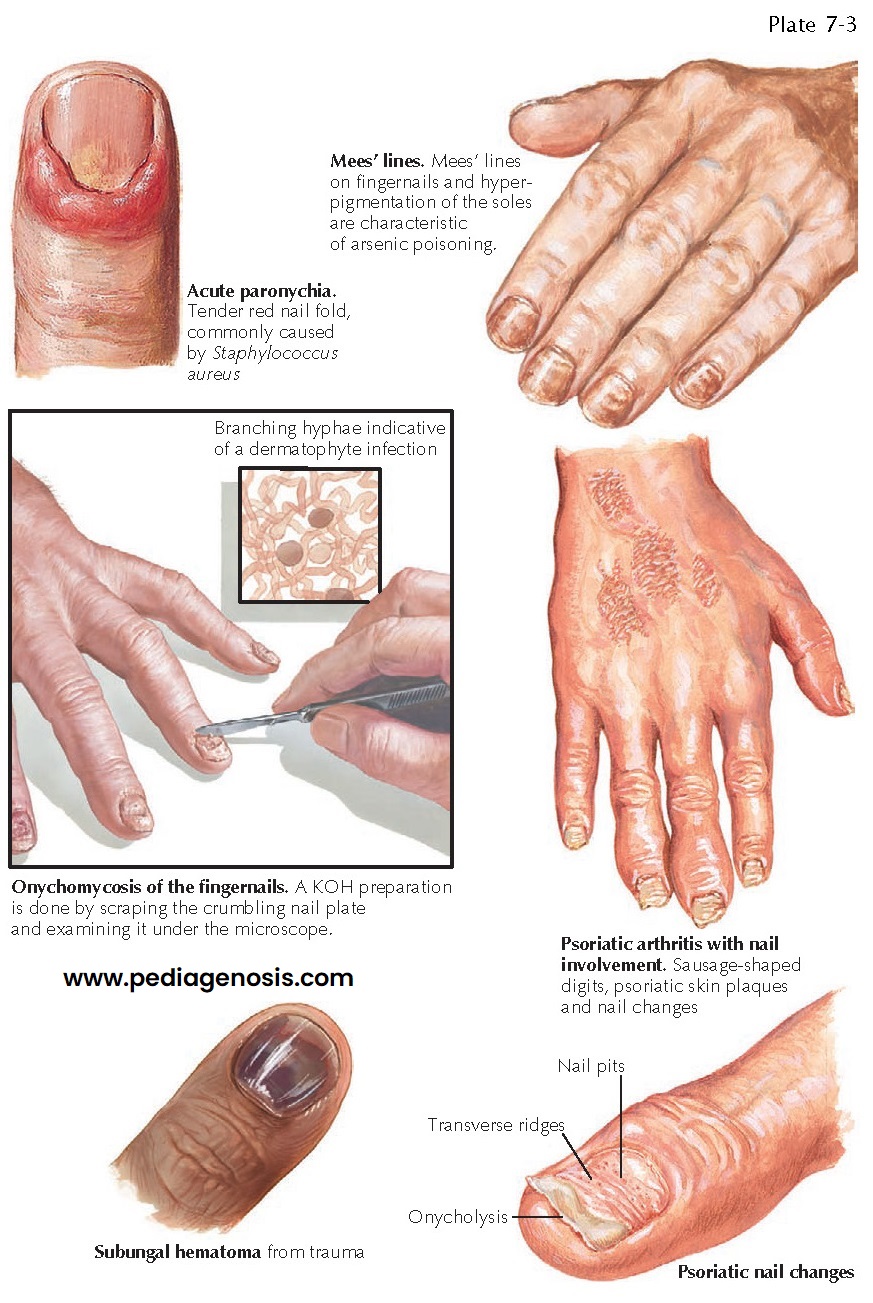
Nail disorders are frequently encountered in the clinical setting. They can occur secondary to an underlying systemic disorder or as a primary disease of the nail unit. The nail unit consists of the nail matrix, bed, and plate and the proximal and lateral nail folds. Disorders of the nail plate and nail bed can manifest in a variety of ways. Systemic disease can manifest through changes in the nail unit. Beau’s lines and Mees’ lines of the nail are two nail findings seen in systemic disease. Beau’s lines are caused by a nonspecific halting of the nail matrix growth pattern, and Mees’ lines are specific for heavy metal toxicity. Dilation of the capillaries of the proximal nail fold or cuticular erythema can be a sign of connective tissue disease. The complete skin examination should also include an examination of the nails, because they offer insight into the patient’s health.
One
of the most serious nail unit disorders is melanoma of the nail matrix.
Melanoma may manifest as a linear, pigmented band along the length of the nail.
As time progresses, the proximal nail fold and hyponychium may also become
pigmented and involved with melanoma. The finding of pigment on the proximal
nail fold has been termed Hutchinson’s sign. This sign is not seen in
subungual hematomas. All new pigmented nail streaks should be evaluated and a
biopsy considered. The biopsy requires nail plate removal and retraction of the
proximal nail fold. The biopsy of a pigmented nail streak is performed within
the nail matrix. Biopsies of the nail matrix may lead to a thinner nail or to
chronic nail dystrophy due to disruption of the matrix. Subungual melanoma
tends to be diagnosed late, because these tumors are easily overlooked or
passed off as a subungual hematoma. It is critically important to differentiate
the two.
Subungual
hematomas are frequently encountered. Most are caused by direct trauma to the
nail plate and nail bed, which causes bleeding between the plate and bed. Acute
hematomas can be very painful. Most acute subungual hematomas are on the
fingers and are caused by a crush injury or by a direct blow to the nail plate.
As the blood accumulates under the nail plate, the pressure created can cause
excruciating pain. This can be easily treated by nail trephination. A
small-gauge hole is bored into the overlying nail plate with a hot, thin metal
object or small drill. Once the nail plate has been punctured, the blood that
has accumulated under the nail freely flows out of the newly formed channel, and
near-immediate pain relief is achieved. Most traumatic injuries to the nail
unit do not cause these very painful hematomas but rather cause small amounts
of blood to accumulate under the nail plate. Pain is absent or minimal. Most
people remember some trauma to the nail, but others do not. This form of
subungual hematoma can involve small portions of the nail or the entire nail.
There is often a blue, purple, and red discoloration of the underlying nail.
Occasionally, the nail plate has a black appearance and is easily confused with
subungual melanoma. The history can be misleading in these cases, because many
patients with and without melanoma remember some form of trauma to the nail
that might lead the clinician to pass the lesion off as a subungual hematoma.
If any doubt about the diagnosis exists, a nail biopsy should be considered.
The nail plate is removed, and a subungual hematoma is easily distinguished
from a tumor. Most subungual hematomas slowly grow outward toward the distal
free edge of the nail. As the nail grows, its most proximal portion appears
normal. The entire subungual hematoma eventually grows out and is shed or
clipped off once it passes the hyponychium.
Onychocryptosis
(ingrown nail) is almost universally seen in the great toenail. It is caused by
burrowing of the lateral portion of the nail plate into the lateral nail fold.
As the nail punctures the lateral nail fold, it sets off an inflammatory
reaction that causes edema, redness, pain, and occasionally purulent drainage.
Secondary infection is common. Ambulation may become difficult because the pain
forces the patient to avoid pressure.
The
exact etiology of onychocryptosis is not entirely known, but it is believed to
be caused, or at least made more likely, by improper trimming or removal of the
lateral portion of the nail. If the nail plate is cut at varying angles or torn
from its bed by picking, this may allow for the lateral free edge of the nail
plate to enter into the lateral nail fold. Tight-fitting shoes have also been
implicated as increasing the likelihood of developing ingrown nails. This
condition is seen more frequently in young men, but it can be seen in all age
groups. The fingernails are rarely affected. Treatment consists of lateral nail
plate removal with or without a lateral nail matrixectomy. After proper
anesthesia, a nail plate elevator is used to free the involved portion of the
nail. A nail splitter is then used to remove the lateral third of the nail. The
freed nail is grasped with a nail puller, and the nail is removed with a
gentle, back-and- forth rocking motion. The portion of the nail that is removed
from under the lateral nail fold is often larger than expected. Recurrent
ingrown nails usually should be treated with nail matrixectomy. This destroys
the lateral third of the nail matrix, eliminating the ability to form that
portion of the nail and removing the potential nidus from causing further
problems in the future. Application of phenol to the nail matrix after nail
plate avulsion is one of the best methods for destroying the nail matrix.
Bilateral nail fold involvement on the same toe is not infrequently
encountered, and the entire nail can be removed in these cases. Onychocryptosis
is not a primary infection of the nail unit, and any infection is believed to
be secondary to the massive inflammatory response. This is in stark contrast to
an acute paronychia.
 |
| COMMON TOENAIL DISORDERS |
Paronychia
is a nail fold infection with either a bacterial agent (as in acute paronychia)
or a fungal agent (in chronic paronychia). Acute paronychia manifests with
redness and tenderness of the nail fold. The redness and edema continue to
expand, causing pain and eventually purulent drainage. Removal of the cuticle
or nail fold trauma may lead to an increased risk for this infection. Staphylococcus
aureus and Streptococcus species are the most frequent etiological
agents. Chronic paronychia typically is less inflammatory and manifests with
redness and edema around the nail folds. Many digits may be involved. At
presentation, patients typically report that they have been having difficulty
for longer than 6 to 8 weeks. Tenderness is much less significant than in acute
paronychia. Chronic paronychia is usually caused by a fungal infection of the
nail fold with Candida albicans. Individuals who work in occupations in
which their hands are constantly exposed to water are at higher risk for
chronic paronychia. Therapy includes topical anti-fungal and antiinflammatory
agents.
A
felon is often confused with acute paronychia, but it is a soft tissue
infection of the fingertip pulp. It may arise secondary to an acute paronychia.
The clinical findings are those of a swollen, red, painful finger pad. The
treatment is surgical incision and drainage together with oral antibiotics to
cover S. aureus and Streptococcus species.
Onychomycosis
is seen frequently in individuals of all ages, and its prevalence increases
with age. Patients can present with different variants of onychomycosis. The
most frequent type is the distal and lateral subungual onychomycosis. Other
variants include white superficial onychomycosis and proximal subungual
onychomycosis. Trichophyton rubrum is the most frequent cause of all
except white superficial onychomycosis, which is caused most often by Trichophyton
mentagrophytes. Superficial white onychomycosis manifests with a fine,
white, crumbling surface to the nail.
When
it is curetted off, the white areas of fungal involvement are found to affect
only the outermost portion of the nail plate. The material is a combination of
fungal elements and nail keratin. Therapy includes curetting the white involved
portion of the nail and applying a topical antifungal agent for at least 1
month. Distal and lateral subungual onychomycosis manifests with thickened,
yellow, dystrophic appearing nails with subungual debris. There are varying
amounts of onycholysis (nail plate lifting off the nail bed). One nail may be
solitarily involved but it is more common for several nails to be involved and
for the surrounding skin to be involved with tinea manuum or tinea unguium.
Fungal nail infections are much more frequently seen on the toenails than on
the fingernails. The nails can become painful, especially with ambulation.
Occasionally, the entire nail is shed as a result of significant onycholysis,
and the nail that regrows will again be involved with onychomycosis. The thick
and dystrophic nails may become a passage for bacterial invasion of the body.
This is especially true in patients with diabetes. Bacteria can gain entrance
into the skin and soft tissue via the abnormal barrier between nail and nail
fold, and this can lead to paronychia, felon, and the most serious
complication, cellulitis. Distal and lateral subungual onychomycosis almost
always needs to be treated with an oral antifungal medication for any chance of
a cure. Topical agents may be helpful in limited nail disease, but their use is
typically limited to an adjunctive role. Oral azole antifungals, griseofulvin,
and terbinafine have all been used, with similar results. Psoriasis can affect
the nails in many ways. Nail involvement appears more frequently in patients
with severe disease and in those with psoriatic arthritis. The nails can show
oil spots, pitting, ridging, onycholysis, and onychauxis (subungual
hyperkeratosis). The oil spots are represented by a brownish to yellowish discoloration under the nail plate and associated onycholysis. The discoloration
is caused by deposition of various glycoproteins into the nail plate. Nail
pitting can be seen in other conditions besides psoriasis, such as alopecia
areata; it is caused by parakeratosis of the proximal nail matrix, which is
responsible for producing the dorsal nail plate. Ridging and onychauxis is
caused by the excessive hyperkeratosis of the nail bed, which is directly
caused by psoriasis. Therapy for psoriatic nails can involve intralesional
steroid injections or use of systemic agents to decrease the abnormal immune response that
is driving the psoriasis. Onychogryphosis (“ram’s horn” nail deformity)
manifests with an unusually thickened and curved nail that takes the shape of a
ram’s horn.
A
plethora of nail changes may be seen in response to systemic disease. Beau’s
lines are horizontal notches along the nails that may be caused by any major
stressful event. The stressful event typically is induced by prolonged
hospitalization, which causes temporary inadequate production of the nail bed
by the nail matrix. It is entirely corrected spontaneously as the individual
improves. Mees’ lines are induced by heavy metal toxicity, most commonly from
arsenic exposure. They appear as a single, white horizontal band across each
nail. Mees’ lines have also been reported in cases of malnutrition. Terry’s
nails is the name given to nail changes seen in congestive heart failure and
cirrhosis of the liver: More than two thirds of the proximal nail plate and bed
appear dull white with loss of the lunula. Half-and-half nails, also called
Lindsay’s nails, are seen in patients with chronic renal failure. The proximal
half of the nail is normal appearing, whereas the distal half has a brown
discoloration. Yellow nail syndrome manifests with all 20 nails having a
yellowish discoloration and increased thickness of the nail plate. This syndrome
is almost always seen in association with a pleural effusion, often secondary
to a lung-based malignancy.
Koilonychia is one of the most easily recognized deformities of the nail; it is caused by iron deficiency. The nail plate develops a spoon-shaped, concave surface. Splinter hemorrhages may be a sign of bacterial endocarditis. Clubbing, which is defined as loss of Lovibond’s angle, is typically caused by chronic lung disease. The nail unit can manifest disease in many ways, and awareness of the various nail signs can help the clinician diagnose and treat these conditions.





