Cardiovascular
Examination
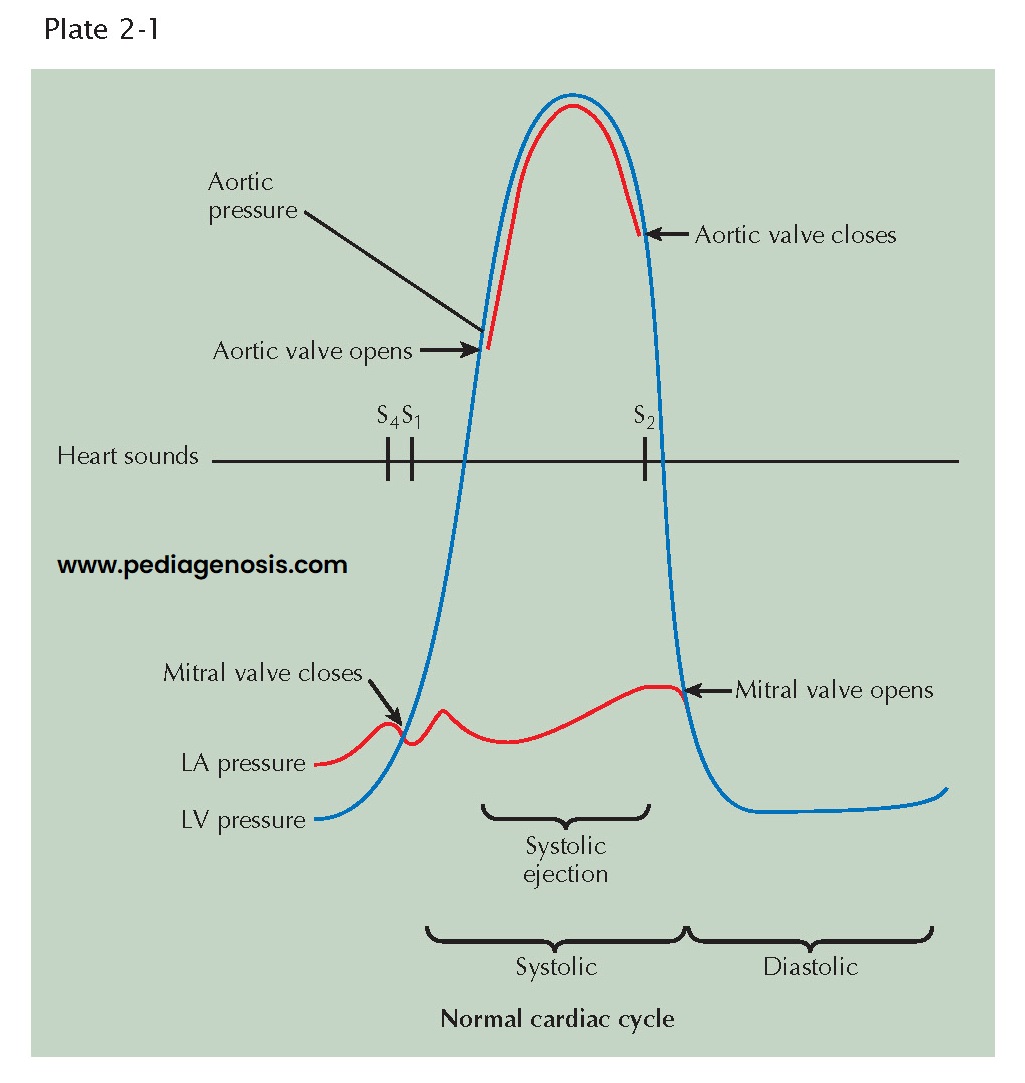 |
| EVENTS IN THE CARDIAC CYCLE: LEFT VENTRICLE |
EVENTS IN THE CARDIAC CYCLE: LEFT VENTRICLE
The events occurring during the cardiac cycle are driven by the left ventricular (LV) pressure. The mitral valve closes and results in the first heart sound (S1) when LV pressure rises above left atrial (LA) pressure (see Plate 2-1). The aortic valve opens when LV pressure rises above aortic diastolic pressure and is the onset of systolic ejection. The aortic valve closes and produces the second heart sound (S2) when LV pressure falls below aortic pressure and terminates systolic ejection. The mitral valve opens when LV pressure falls below LA pressure. The fourth heart sound (S4) occurs in late diastole following atrial contractions.
Cardiac auscultation
is not the only way to examine the cardiovascular system. Peripheral vessels reflect
what is occurring in the cardiovascular system; for example, carotid and femoral
artery examination can reveal peripheral vascular disease. Bruits over these vessels may indicate carotid stenosis
or aortofemoral stenosis. An abdominal bruit may indicate renal artery
stenosis. A decrease in blood pressure in either arm suggests subclavian artery
stenosis. If the ankle-brachial index (ratio of systolic pressure in arm to systolic pressure in ankle using Doppler technique) is less than 0.9, some peripheral
artery disease may be present.
Jugular venous pulsations
seen when the patient is lying with the upper body elevated to 30 degrees suggests
elevated RA pressure of several causes.
Precordial palpation
before auscultation of the heart can help the examiner make the proper cardiac
diagnosis. The apical impulse can suggest LV hypertrophy (enlargement) if sustained
and slow rising. Palpation along the left sternal border may reveal a parasternal
lift, which suggests an elevated right ventricular (RV) pressure of about 40 mm
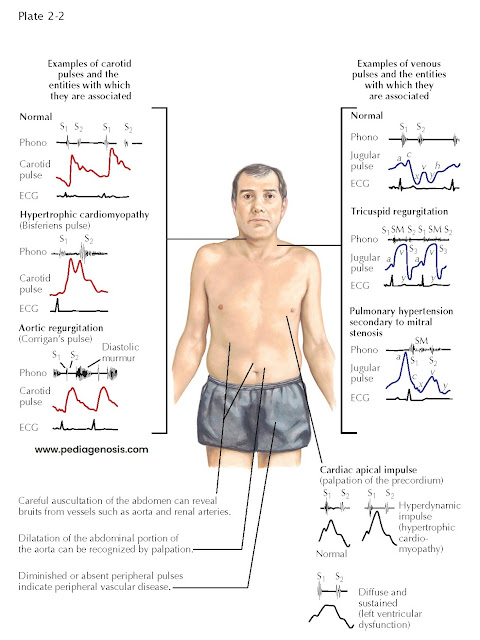
Hg. Plate 2-2 illustrates some examples of carotid pulses and venous pulsations
and cardiac apical impulses associated with specific cardiac disease states.
The basic instrument
of auscultation is the human ear. Although the stethoscope has technical advantages,
it often distorts, decreases, or selectively emphasizes certain vibrations.
Frequently, the naked ear is superior to the stethoscope in the detection of low-pitched
vibrations (S3, S4) because the ear is a larger collector
of sound and fuses auditory with palpatory perception.
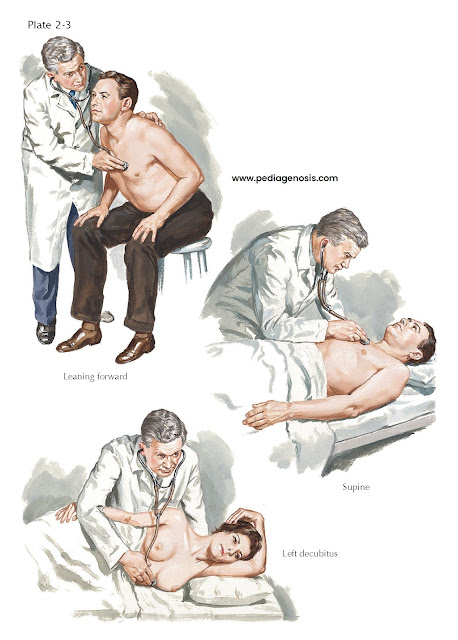
POSITIONS FOR
CARDIAC AUSCULTATION
In auscultation,
various patient positions can be used (see Plate 2-3). The patient may be sitting,
supine, lying on the left side, or bent forward to increase the contact of the apex
with the chest wall, as preferred for mitral or LV sounds and murmurs. The left
side (left decubitus) position accentuates the rumbling murmur of mitral stenosis.
The bent-forward position is preferred for aortic diastolic murmurs, whereas the
supine position is best for pulmonic and tricuspid murmurs.
AREAS OF CARDIAC
AUSCULTATION
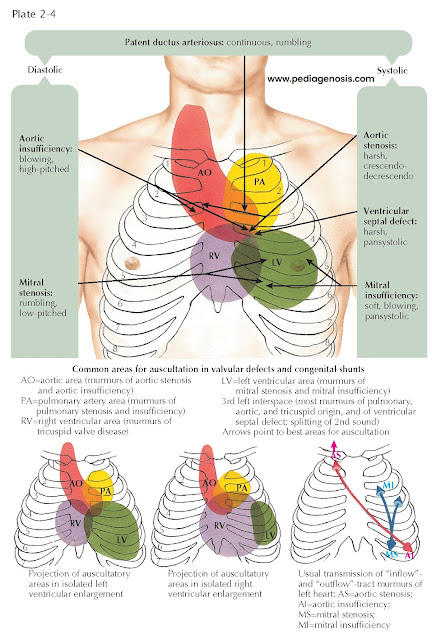
The conventional
designations for areas of auscultation have been mitral, tricuspid, aortic, and
pulmonary. Current understanding divides the thorax into seven areas: left
ventricular, right ventricular, left atrial, right atrial, aortic, pulmonary, and
descending thoracic aortic (see Plate 2-4).
Left Ventricular
Area
The apical area
(“mitral” area) is the best location for detecting not only the murmur of mitral
stenosis or insufficiency but also the LV or atrial gallops and the aortic component
of the second sound (A component of II). The murmurs of aortic stenosis and
especially of aortic insufficiency also are often heard well at this location. However,
these vibrations are detected over a larger area formed by the entire left ventricle,
centering around the apical beat and extending to the fourth and fifth left interspaces
medially and to the anterior axillary line laterally. In patients with ventricular
enlargement, the sound shifts to either the left or the right.
The “tricuspid”
area is renamed the right ventricular area. In addition to the murmurs of tricuspid
stenosis and insufficiency, RV and atrial gallops and the murmurs of pulmonary insufficiency
and ventricular septal defect can be well heard here. The RV area includes the lower
part of the sternum and the fourth and fifth interspaces, 2 to 4 cm to the left
and 2 cm to the right of the sternum. This area may extend also to the point of
maximal impulse, in the presence of severe RV enlarge- ment; the “apex” in such
patients is formed by the right ventricle.
The aortic component of S2 and the murmurs of aortic
valve defects are often heard well at the third left interspace (Erb’s area). This
point is frequently more revealing
than the second right interspace, except in patients with dilatation of the ascending
aorta, where the manubrium or the second right interspace
may be more informative. The aortic area should designate both the aortic root and
part of the ascending aorta. The vibrations heard best in this area include the
murmurs caused by aortic stenosis, aortic insufficiency, augmented flow across the
aorta or dilatation of the ascending aorta, and abnormalities of the neck arteries,
as well as the aortic ejection click and aortic component of S2.
Pulmonary
Area
The pulmonary area
should refer to the pulmonary artery rather than the pulmonary (pulmonic)
valve. The murmurs of pulmonary stenosis and insufficiency, the murmur caused by
increased flow or dilatation of the pulmonary artery, the pulmonary ejection
click, the pulmonary component of the second sound (P component of II), and
the murmur of patent ductus arteriosus are heard best here. The pulmonary area is
formed by the second left interspace near the sternal edge and extends upward to
the clavicle and downward to the third left interspace near the sternal margin.
However, it may also extend posteriorly at the level of the fourth and fifth dorsal
vertebrae.
IMPORTANT COMPONENTS OF CARDIAC EXAMINATION
MOST SIGNIFICANT
AUSCULTATORY FINDINGS
Heart Sounds
The first heart
sound (S1) is often louder over the LV area (apex and midprecordium),
whereas the second heart sound (S2) is frequently louder over
the aortic and pulmonary areas (base). The first sound is a long noise of lower
tonality, whereas the second sound is shorter and sharper.
In normal adolescents
or young people, S1 may be split. The best area for hearing this split
sound is at the third left interspace. This splitting is not influenced by respiration.
The loudness of S1 is decreased in myocarditis, myocardial infarction
(MI), myocardial fibrosis, hypothyroidism, mitral insufficiency (soft), aortic
insufficiency, and pericarditis with effusion. S1 is increased in mitral
stenosis, systemic hypertension, and hyperthyroidism.
The second sound
is frequently split during inspiration and in normal children and young people.
The best area for hearing this splitting is the third left interspace, close to
the sternum (Erb’s point). S2 has an increased loudness of the aortic
component in systemic hypertension, coarctation of the aorta, and aortitis. Decreased
loudness of S2 characterizes aortic stenosis. The aortic component may
be so delayed as to follow the pulmonary component, a paradoxical splitting. S2
has increased loudness of the pulmonary component in pulmonary hypertension, whereas
loudness is decreased in pulmonary stenosis. The pulmonary component not only is
smaller but also is delayed, causing a wider splitting. S2 has wider,
fixed splitting in conditions presenting a diastolic overload of the right side
of the heart and in right bundle branch block, because of a delay in the
pulmonary component. Patients with left bundle branch block may present with such
a delay in the aortic component as to cause paradoxical splitting.
 |
| POSITIONS FOR CARDIAC AUSCULTATION |
The third
heart sound (S3) may be normal in children, adolescents, and young
athletes but may be audible over the LV or RV area in ventricular overload,
myocarditis, tachycardia, or heart failure.
The fourth heart
sound (S4) is not heard in the normal heart. S4 is audible
over the LV area in hypertension, during myocardial ischemia, or when the ventricle
is stiff and noncompliant, as in diastolic dysfunction. S4 can also be
heard in patients with ventricular volume overload, myocarditis, tachycardia, atrial
flutter, and complete or incomplete atrioventricular (A-V) block or
obstruction. The fourth sound is then called atrial gallop. A left atrial
gallop is frequently heard in aortic stenosis or systemic hypertension. A right
atrial gallop is often heard in pulmonary stenosis or pulmonary hypertension. A
slightly different type is the summation gallop, caused by the summation
of S3 and S4. This is most often seen in patients with tachycardia
and grade 1 A-V block.
A systolic ejection
click can be heard over either the pulmonary area (pulmonary ejection sound)
or the aortic area (aortic ejection sound). These clicks are caused by “doming”
of the aortic or pulmonary valve; the aortic valve may be bicuspid. These ejection
sounds occur with dilatation of the aorta or pulmonary artery or narrowing of the
aortic or pulmonary valve, usually with poststenotic dilatation. The ejection click
is a high-frequency sound due to abrupt halting of the valve opening.
A diastolic opening snap can be heard in the fourth left interspace,
close to the sternum, over the entire LV area, or even over the entire precordium,
in patients with a pliable noncalcified valve. This is the mitral opening
snap most often heard in mitral stenosis. Occasionally it can be heard in diastolic
overload of the left side of the heart (mitral insufficiency, patent ductus). A
tricuspid opening snap is audible over the RV area in patients with tricuspid
stenosis and occasionally can be heard in diastolic overload of the right ventricle
(tricuspid insufficiency, atrial septal defect).
Murmurs
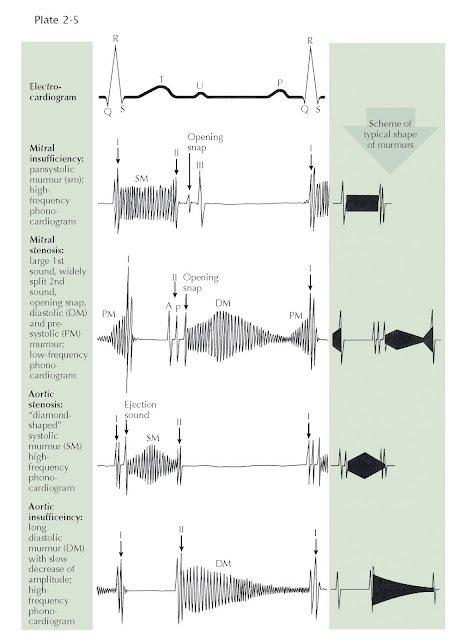
The regurgitant
murmur of A-V valve insufficiency is holosystolic and usually loud (see Plate
2-5). The murmur of mitral insufficiency is maximal over the LV area and easily
audible at the left axilla, whereas the murmur of tricuspid insufficiency is maximal
over the RV area and is well heard over the right precordium. Inspiration or
inspiratory apnea increases the loudness of the tricuspid murmur but decreases the
loudness of the mitral murmur.
The murmur of A-V
valve stenosis is a typical, low-pitched rumble which acquires higher pitch
and greater loudness in presystole (presystolic accentuation) if there is sinus
rhythm. It is heard best in mitral stenosis in the fourth left intercostal space,
halfway between the apex and the sternal border. In tricuspid stenosis this rumble
is heard best over the RV area. This murmur becomes louder in inspiration because
of increased flow across the tricuspid valve during inspiration.
The regurgitant
murmur of semilunar valve insuffici ncy is a high-pitched, blowing, occasionally
musical decrescendo. In aortic insufficiency the murmur is loudest in the third
left interspace (Erb’s area), and can be followed along the left sternal border
toward the apex. If the ascending aorta is dilated, the murmur is louder in the
second right interspace and can be fol- lowed downward along the right sternal border.
In pulmonary insufficiency the murmur is loudest over the second left interspace
and can be followed downward from the upper left to the lower right part of the
sternum. If the patient has pulmonary hypertension, the murmur sounds similar to
aortic regurgitation. If the pulmonary artery pressure is normal or low, the
murmur may have a rumbling character.
The stenotic
murmur of the semilunar valves is the loudest of all murmurs. It is harsh,
starts slightly after S1 with aortic valve opening, and is often preceded
by an ejection click, especially if the valve is bicuspid
and mobile. The murmur often has a crescendo-decrescendo quality and ends before
or with S2, depending on the severity of the stenosis. In aortic
stenosis the murmur is maximal in the third left or second right interspace. It
is readily heard over the suprasternal area and the carotid arteries and can be
heard at the apex. In subvalvular aortic stenosis, it is maximal over the LV area.
In pulmonary stenosis the murmur is best heard over the pulmonary area. It radi-
ates moderately downward and often can be heard in the back over the lungs.
The murmur caused
by a ventricular septal defect is long, harsh, and pansystolic. It is heard best
over the RV area.
The murmur caused
by patency of the ductus arteriosus is a continuous, machinery-like murmur because
aortic systolic and diastolic pressures are higher than pulmonary systolic and diastolic
pressures. It is best heard over the first and second intercostal spaces.
 |
| MURMURS |
Friction Rubs
Friction rubs can be heard over various areas and resemble the sound made by rubbing new leather. Friction rubs can be heard in atrial systole, ventricular systol , and ventricular diastole (i.e., threecomponent rub).