PREECLAMPSIA
I—SYMPTOMS
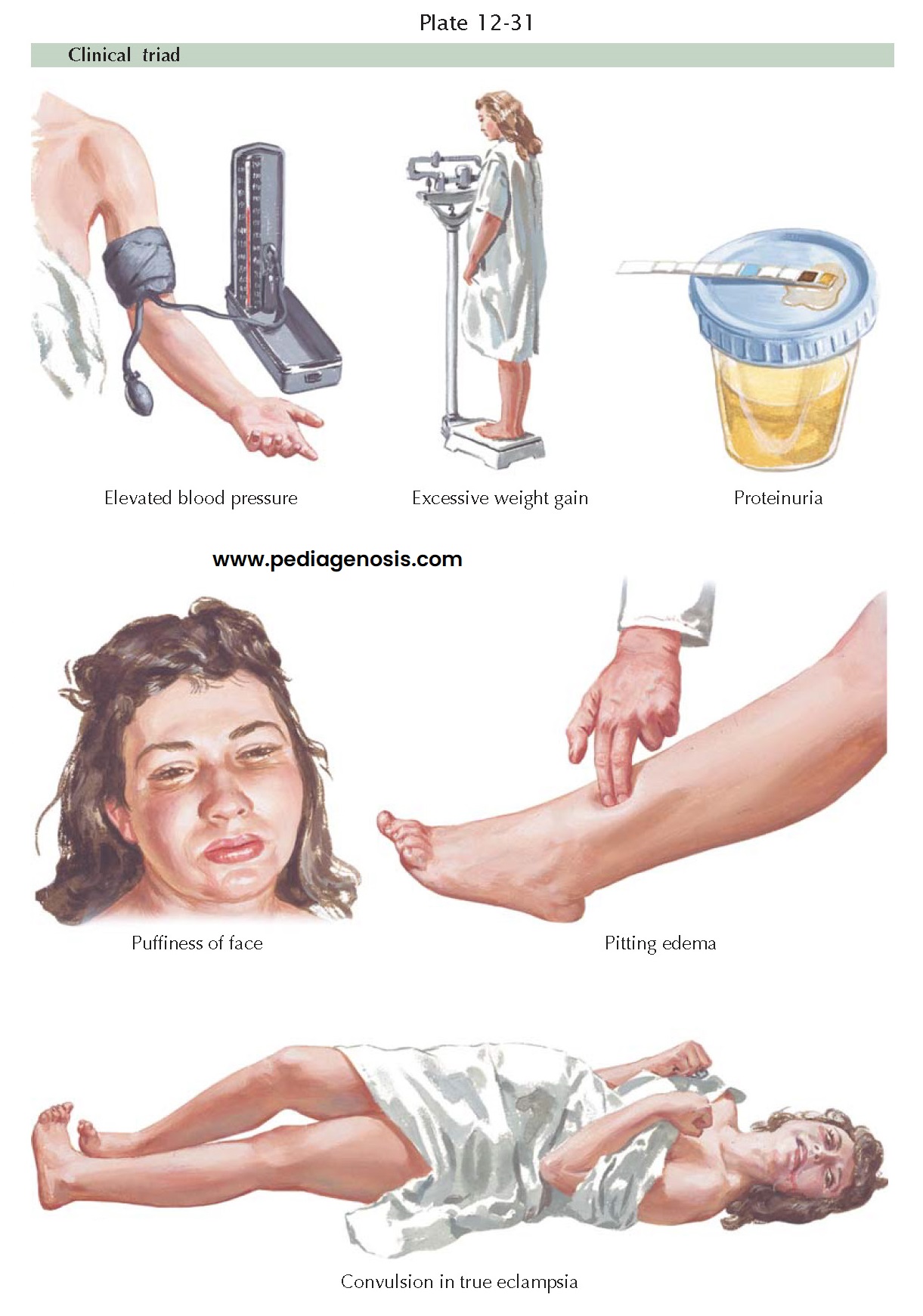
Preeclampsia (once called toxemia of pregnancy) is a
pregnancy-specific syndrome occurring after 20 weeks’ gestation. It involves
reduced organ perfusion, vasospasm, and endothelial activation and is
characterized by hypertension, proteinuria, and other symptoms. Pregnancy can
induce hypertension or aggravate existing hypertension. Edema and proteinuria
(one or both) are characteristic pregnancy-induced changes. If pre-eclampsia is
untreated, convulsions (eclampsia) may occur. Chronic hypertension may be
worsened by being superimposed on pregnancy-induced changes. Severe cases may
include hemolysis, elevated liver enzymes, and low platelet counts, labeled
HELLP syndrome, which occurs in up to 20% of severe preeclampsia. Preeclampsia
occurs in 5% to 8% of all births (250,000 cases per year) and results in 150
maternal deaths and 3000 fetal deaths per year. (Overall, hypertensive disease
of some type occurs in approximately 12% to 22% of pregnancies, and it is
directly responsible for 17.6% of maternal deaths in the United States.)
In the great majority of cases, the clinical manifestations of preeclampsia occur after the 20th week of gestation and disappear following delivery. Preeclampsia before 20 weeks’ gestation may occur with gestational trophoblastic neoplasia and antiphospholipid antibody syndrome. Another uncommon presentation for pre-eclampsia is in the postpartum period, when it has been reported to occur up to 7 days after delivery.
The earliest clinical
signs of preeclampsia are often sudden and excessive weight gain, accompanied
by a blood pressure higher than 140/90 mmHg and by proteinuria. Such weight
gain reflects the retention of water and electrolytes. Eventually, pitting
edema, particularly in the legs and face, develops. However, before the stage
of pitting edema is reached, the interstitial space may accumulate large
quantities of fluid. The normal average weight gain during pregnancy does not
exceed 2½ to 3 lb per month, and a greater weight gain should be suspected as
abnormal water retention. Edema may precede hypertension, but for the clinical
diagnosis of preeclampsia, the increased blood pressure is essential. In this
respect the elevation of the diastolic blood pressure is more significant than
that of the systolic, because it is the former which reflects the status of the
peripheral resistance.
The criteria needed to
diagnose a patient with pre-eclampsia include the results of 24-hour urinary
protein measurement that demonstrate >300 mg of protein in 24 hours. In
addition, these patients have blood pressure measures above 140/90 mm Hg. These
patients also have characteristic renal glomerular lesions (capillary
endotheliosis) and increased vascular reactivity. They often manifest elevated
liver enzymes, and thrombocytopenia. In the past, hypertension indicative of
preeclampsia has been defined as an elevation of more than 30 mm Hg systolic or
more than 15 mm Hg diastolic
above the patient’s baseline pressure; however, this has not proven to be a
good predictor of outcome and is no longer part of the criteria for
preeclampsia, though these patients do require close monitoring. Pre-eclamptic
patients may undergo convulsions with only moderate blood pressure elevation
and only a slight degree of edema.
Conscientious, regular prenatal care is important in order to detect signs of preeclampsia as early as possible. The onset of preeclampsia may be insidious or abrupt. The patient may feel well and not be aware of abnormal weight gain, proteinuria, or rising blood pressure. There may be a sudden progression into the convulsive phase, necessitating the termination of the pregnancy, thereby resulting in prematurity of the infant, which is the most frequent cause of perinatal mortality in preeclampsia. It is thought that severe preeclampsia predisposes to chronic hypertensive vascular disease, and the incidence of severe preeclampsia in subsequent pregnancies is increased.