Pediatrics:
Disruptive Behavior Disorders
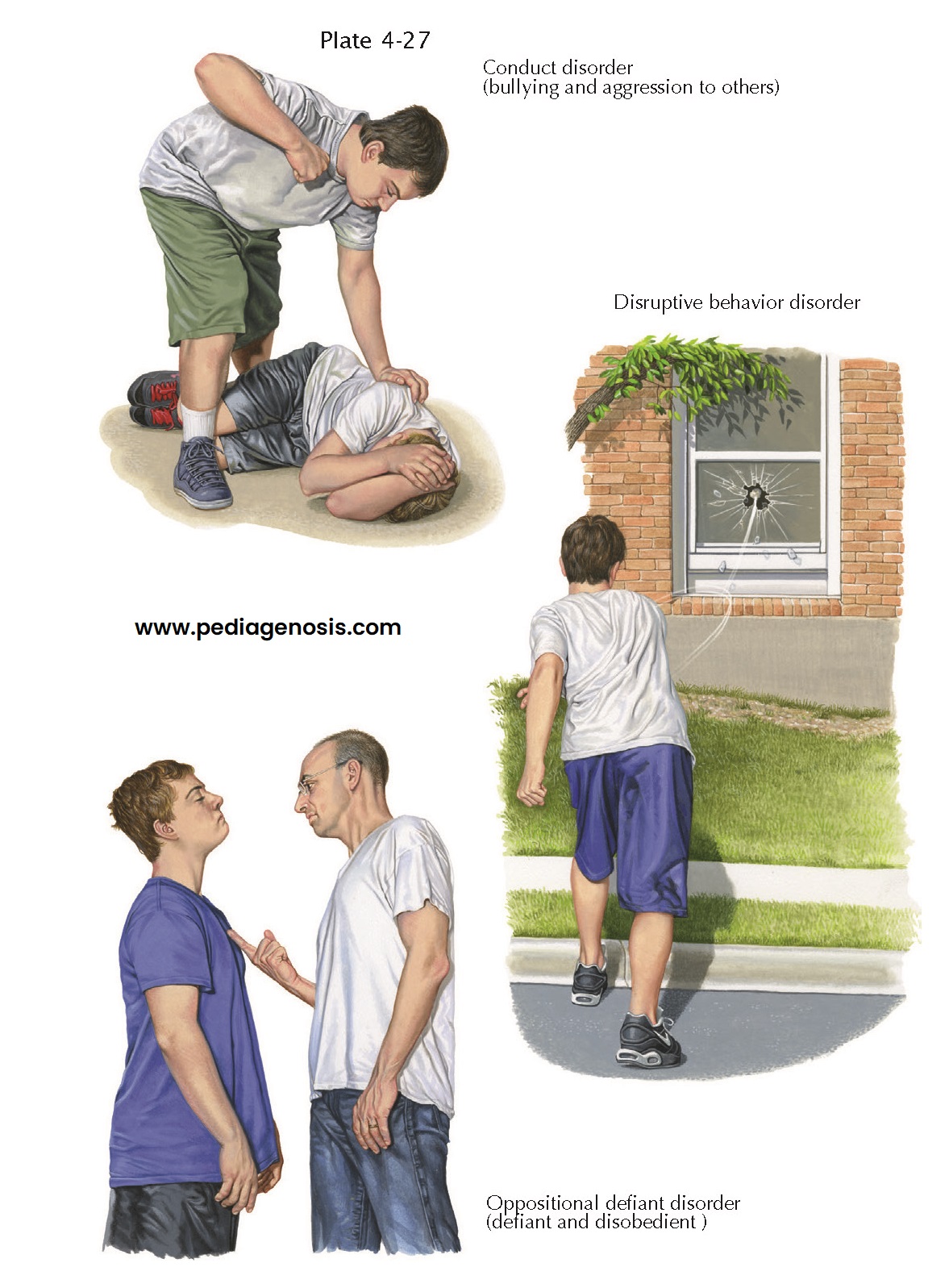
The disruptive behavior disorders (DBDs) are
mental health problems occurring in children and adolescents, more commonly in
boys, characterized by out-of-control behavior. Prevalence rates vary from 1%
to 16%. A cluster of factors, including the child’s characteristics, parental
interactions, and environmental factors contribute to their development.
Ineffective parenting strategies often underlie these disorders. Parents may have insufficient time and emotional energy for the child or may use inconsistent methods of disciplining and limit setting. These ineffective strategies include authoritarian parenting, wherein the parent demonstrates too much anger or is too harsh, and permissive parenting, with the parent giving in to the child’s excessive demands. Authoritative parenting is defined as having high levels of both warmth and firmness and is the most effective parenting strategy.
The DBD child may be
strong-willed because of genetically inherited personality characteristics,
certain intrauterine exposures (such as cigarette smoking), lack of positive
parental attachment, because of stress, or a lack of predictable structure in
the home or com- munity environment. Disruptive behavior disorders are more common
in families with serious marital discord, families of low socioeconomic status
and in neighborhoods characterized by high crime rates and social
disorganization.
Oppositional
Defiant Disorder. Oppositional
defiant disorder is the less severe. It is characterized by a recurrent pattern
of negativistic, defiant, disobedient, and hostile behavior, such as
deliberately annoying others, frequent arguments, and angry outbursts directed
toward authority figures, that is, parents and teachers. To confirm the diagnosis,
these behaviors must be more frequent and more severe than normal children
exhibit, present at least 6 months and impair the youth’s function at home, at
school, or with peers.
The more serious DBD—conduct
disorder—is characterized by a persistent pattern of serious rule-violating
behavior, including instances that harm or have the potential to harm others.
Physical aggression to people and animals, destruction of property, lying or
stealing, running away from home, and truancy are typical examples. Boys are
more likely to have conduct disorder compared with oppositional defiant
disorder. Rather than physical aggression, girls are more prone to use verbal
attacks, ostracism, or character defamation. To confirm this diagnosis, DBDs
must be present at least 1 year, impairing the youth’s home, school, and/or
peer function.
Diagnosis. DBDs are most accurately diagnosed by
child and adolescent psychiatrists, child psychologists, child-trained social
workers, and clinical nurse specialists. The evaluation requires input from
multiple individuals who know the child. The diagnosis is based upon findings
from interviews and a mental status examination. There are no specific
diagnostic imaging studies, blood tests, or other medical tests that are
diagnostic.
Treatment. The best therapy for oppositional
defiant disorder is helping the parent learn effective parenting strategies.
Treatment goals include helping the youngster become more cooperative and less
argumentative or destructive. It is very useful to ascertain the child’s and
family’s strengths and build on them in addition to focusing on their problems.
Behavior modification strategies
include developing a warm, loving relationship between parent and child;
providing a predictable, structured environment; setting clear and simple
house-hold rules; consistently praising and rewarding positive behaviors (such
as completing chores or homework); consistently ignoring annoying behaviors
(such as whining or arguing), followed by praise when the annoying behavior
ceases; and consistently outlining potential consequences (such as loss of
privileges) for dangerous or destructive behaviors. Social-emotional skills
training for the child, helps them develop skills to identify and manage
feelings, get along with others, and make good decisions based on thinking
rather than feeling.
Because conduct disorder
is an extremely serious condition, treatment must be more intensive and extensive, sometimes involving other
child-serving agencies (i.e., juvenile justice and child welfare). Treatment is
likely to be effective when administered early in the course of the disorder
before maladaptive behaviors become more entrenched. If physically aggressive
behavior is prominent in conduct disorder, medications (including atypical antipsychotics)
can be helpful.
Course. Oppositional defiant disorder, and to a lesser extent, conduct disorder respond well to the above treatments when delivered by qualified mental health professionals. Although some children grow out of the DBDs, if untreated, these disorders can go on to cause significant problems, including difficult relationships with parents and other adults, failure at school and delinquency, and in adulthood, antisocial or criminal behavior.