OSTEOCHONDRITIS DISSECANS AND
OSTEONECROSIS
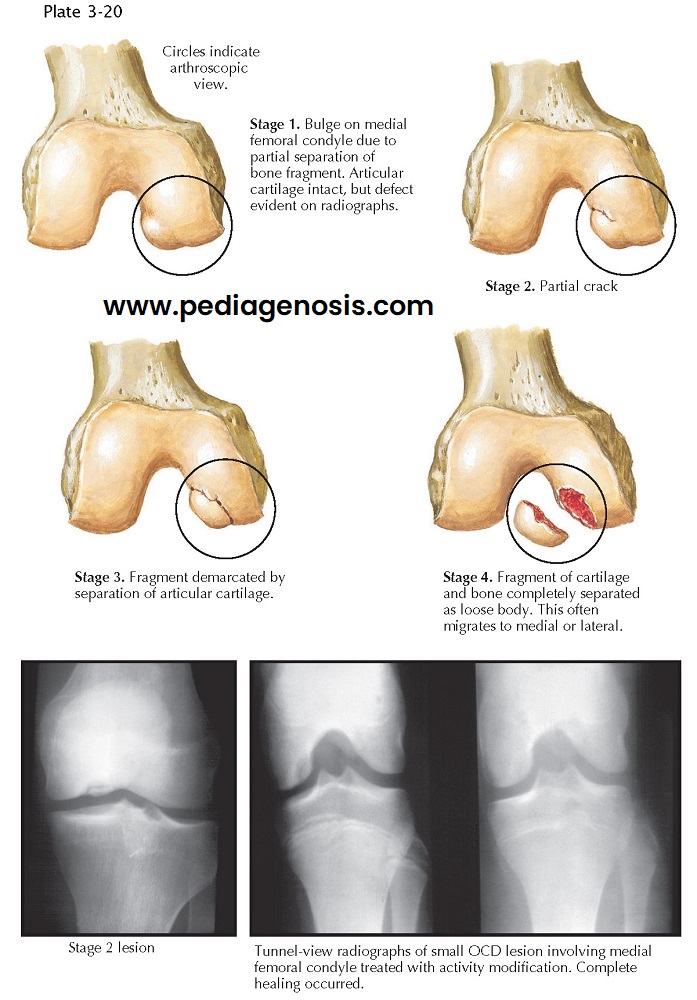
PROGRESSION OF OSTEOCHONDRITIS DISSECANS
Osteochondritis dissecans (OCD) is a defect in the sub- chondral region of the apophysis or the epiphysis of a bone, often with partial or complete separation of the bone fragment. When this occurs in the distal femur, it is a common source of loose bodies in the knee. Whereas OCD most often affects the posterolateral aspect of medial femoral condyle, it can also occur in other regions of the knee, as well as the shoulder, elbow, and foot.
Although trauma is the most likely cause of OCD, a
single event is probably not responsible: this would cause a true fracture if
the force is large enough. Repetitive overloading is thought to affect the
local blood supply, making a region more susceptible to fragmentation and
separation. Trauma is believed to damage the delicate blood supply to the
affected bone in a process similar to Legg-Calvé-Perthes disease of the hip.
Obese children are more prone to this problem because of increased load on
their joints. Normally, the knee joints are subjected to forces up to six times
body weight. Thus, an additional 30 lb of body weight can add about 180 lb in
forces to a joint. It is no wonder that knee problems arise under such
conditions. Fragments may separate from the bone and become loose bodies in the
joint. If the defect is large, the joint may become incongruous, leading to
mechanical signs and symptoms. Whereas the bony lesion is often the center of
attention because of its visibility on radiographs, maintenance of a smooth
overlying articular surface in the weight- bearing region is the most important
prognostic factor. The onset of OCD is frequently insidious, with patients
reporting vague complaints, such as intermittent, poorly localized aching.
Generally, the pain intensifies with exercise but may persist even at rest. The
knee may feel stiff, and floating fragments of bone and cartilage can cause the
knee to catch or lock. If a sufficiently large fragment becomes loose in the
joint and trapped between the condyle and tibia, the patient may feel a sudden pain and the knee may “give way.” These
episodes may produce synovial effusions.
Physical Examination. On physical
examination, forcible compression of the affected side of the knee joint
elicits crepitation during knee flexion and extension. In addition, the
affected femoral condyle will be tender on palpation.
Imaging. Radiographs
are necessary for diagnosis, and the notch view (anteroposterior view with the
knee flexed 90 degrees), tunnel view (angled posteroanterior projection with the knee flexed at 40 degrees), or
lateral view will often best reveal the defect. Bone scans can help
differentiate acute processes from chronic ones. MRI is often used to define
the extent of the defect in both size and detachment from the articular
surface, thereby providing important information for potential surgical
planning.
Treatment. The goal of
treatment is to maintain or reestablish a smooth articular surface and to
remove loose fragments. Conservative measures suffice in the early stages. If the
fragment has not separated from the femoral condyle, the lesion can be
considered stable and protected appropriately with activity and weight-bearing
modification. When defects involve the weight- bearing region of the femur,
walking with crutches to avoid placing full body weight on the affected limb is
essential while symptoms persist. Immobilization is rarely needed and should be
avoided whenever possible, because gentle knee motion is beneficial to the
jeopardized region of the articular cartilage.
A loose or detached fragment can be removed with
arthroscopy. At the same time, drilling through areas of poorly vascularized
bone into regions of good vascularity may induce a vascular healing response.
When the fragment represents a large part of the weight-bearing region or
appears amenable to reduction, internal fixation with Kirschner wires or screws
should be considered. The presence of multiple fragments lessens the chances of
obtaining a congruous surface. These fragments should be removed and the base
of the lesion drilled.
The prognosis for OCD of the knee depends on the age
at which it occurs and the extent of the involvement of the weight-bearing
regions. In short, any process such as this that causes an incongruity in the
very delicate surface of the knee joint predisposes to the development of
osteoarthritis.
Defects that occur in children before the closure of
the growth plate frequently heal well with conservative treatment if the
fragment has not detached; in fact, many cases may go undetected. When
radiographs are taken for other reasons, these defects are not unusual
findings. Prognosis is guarded if the fragment detaches, especially when
leaving a significant defect in the weight-bearing region. Lesions that occur
after closure of the growth plate are less likely to heal.
OSTEONECROSIS
Osteonecrosis is similar to OCD, but in the knee the
diagnosis of osteonecrosis indicates a large lesion that typically occurs in a
female patient older than age 60 years (the female-to-male ratio is 3:1) and
occasionally in a younger patient
with predisposing factors, such as long-term corticosteroid therapy or sickle
cell anemia. These patients often present with acute onset of pain secondary to
a subchondral fracture and collapse of the articular surface. The medial
femoral condyle is most commonly involved, but osteonecrosis also may occur in
the lateral femoral condyle and the tibial plateau (usually medial).
Imaging. Initial plain
radiographs may be normal but eventually show flattening of the articular
surface, subchondral
radiolucency, and sclerosis of surrounding bone. MRI can be used to depict the
involved areas and may be used to detect changes not yet visible in plain
radiographs.
Treatment. Smaller lesions (<5 cm2) typically have a better clinical prognosis and may be satisfactorily treated with activity modification and use of assistive devices such as a cane. Progressive symptoms may necessitate drilling of the lesion, realignment osteotomy, or total knee replacement.