KNEE LIGAMENT INJURY
 |
| RUPTURE OF THE ANTERIOR CRUCIATE LIGAMENT |
Ligament injuries (sprains) of the knee are very common in athletes. In first-degree sprains, the ligament is trenched, with little or no tearing. These injuries produce mild point tenderness, slight hemorrhage, and swelling. Erythema may develop over the painful area but resolves in 2 or 3 weeks after injury. Joint laxity is not present, and the injury does not produce any significant long-term disability. Appropriate treatment consists of rest and muscle rehabilitation. Seconddegree sprains are characterized by partial tearing of the ligament, resulting in joint laxity, localized pain, tenderness, and swelling. When stress is placed on a joint during examination, the examiner should still feel a definite “end point” to the joint movement. Because the ligament is only partially injured, the joint remains stable; thus, vigorous rehabilitation alone will likely be sufficient treatment. Third-degree sprains produce complete rupture of a ligament, making the joint unstable. Tenderness, instability, absence of a definite end point to stress testing, and severe ecchymosis are the hallmarks of third-degree sprains. Surgical intervention may be needed.
Sprains of the medial (tibial) collateral ligament are caused by a valgus force to the knee. Patients
frequently report a snapping or tearing sensation and pain on the medial aspect
of the knee. If only the MCL is injured, patients can usually continue to walk
and may be able to continue the activity that causes the injury.
Physical examination reveals tenderness along the
course of the MCL, and careful palpation can isolate the precise level of
injury: at the origin of the ligament, on the medial femoral condyle, at the
joint line (mid-substance), or along the long distal insertion of the ligament
into the medial aspect of the tibia. Patients are more comfortable if examined
lying supine on the examining table with the thigh supported. The physician
cradles the lower leg in both hands off to the side of the table and
alternately applies varus and valgus stresses to
the knee (varus and valgus stress tests). When the leg is fully extended, the
PCL is the structure most responsible for mediolateral stability. However,
placing the knee in 30 degrees of flexion takes the PCL “out of play” so the
MCL can be tested by applying a valgus force.
Third-degree sprains of the MCL may require direct
surgical repair. However, an isolated third-degree sprain may be successfully
treated by controlling swelling, by
increasing range of motion, and with rehabilitation of the quadriceps femoris
and hamstring muscles.
Marked medial (valgus) laxity may indicate that the
posteromedial corner of the knee capsule is also injured. Surgical repair is
needed to prevent residual rotational instability. A football clipping injury
may result in the “unhappy triad” of O’Donoghue, which includes ruptures of the
MCL and the ACL plus a tear of the medial meniscus. However, in the recent literature it has been shown that the
lateral meniscus is more likely to be acutely torn at the time of ACL injury,
whereas the medial meniscus is more often compromised in the chronically
ACL-deficient knee. These injuries often require arthroscopically aided repair
of the ligaments as necessary and repair of the injured meniscus if possible.
 |
| LATERAL PIVOT SHIFT TEST FOR ANTEROLATERAL KNEE INSTABILITY |
RUPTURE OF THE ANTERIOR CRUCIATE LIGAMENT
The ACL is the primary restraint to anterior
translation of the tibia and it also contributes to internal rotation and
varus/valgus instability with the knee extension. The anatomic configuration of
its two bundles ensures functional tautness throughout the arc of motion, with
the anteromedial bundle taut in flexion and the posterolateral component taut
in extension. Although it may be torn by a contact injury, the ACL is most
commonly injured without contact by a decelerating valgus angulation and
external rotation force. In basketball, the ACL is commonly torn when a player
lands from jumping with the knee in hyperextension and the tibia in internal
rotation. The player hears a “pop,” feels a tear and acute pain in the knee,
and may not be able to continue playing. The knee may feel very unstable during
weight bearing and is often felt as a “giving way” of the knee. Patients
complain that their knee slips or slides when they turn right or left with the
foot planted. This sliding reflects the tibia subluxating anteriorly on the
femur. Rupture of the ACL is a common cause of acute traumatic hemarthrosis.
Physical Examination and Special Tests
·
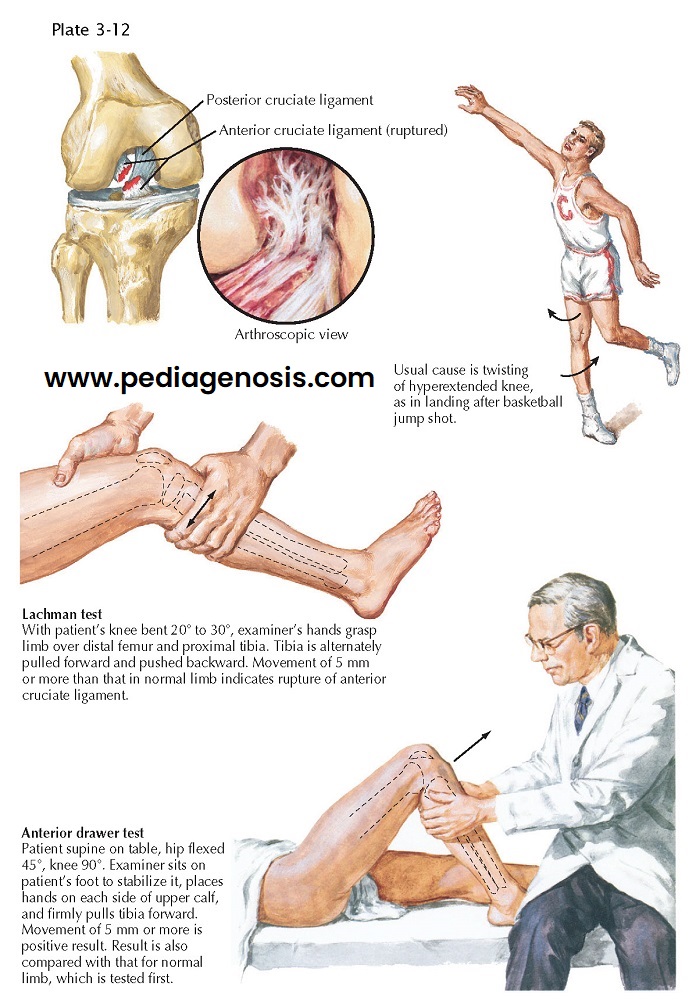
Lachman test: This test is simple to perform and relatively painless for the patient
with an acute injury. The examiner compares the amount of play in the injured
knee with that in the normal one to deter- mine if abnormal motion is present.
The Lachman test is performed with the knee flexed 20 degrees to reduce the
stability provided by the menisci. One of the examiner’s hands stabilizes the
femur while the other hand grasps the proximal tibia. With the patient relaxed,
the examiner attempts to slide the proximal tibia anteriorly on the femur. An
intact ACL prevents the tibia from sliding forward. When the ligament is injured, the tibia is moved from its
normal position and can be subluxated anteriorly during the test. The examiner
must note the quality of the end point of this stress test. If there is a solid
mechanical stop at the most anterior extent of tibial motion, the ACL may be
only partially torn. However, if the end point is soft and spongy, a complete
rupture should be suspected. The integrity of the PCL must be ascertained before the result of this test can be
considered valid. If the PCL is ruptured, the proximal tibia sags posteriorly,
and the Lachman test will seem to be positive as the posterior subluxation is
reduced.
·
Anterior drawer test: The anterior drawer test is performed with the patient lying supine,
resting comfortably with the knee flexed 90 degrees (see Plate 3-12). The patient’s foot is stabilized during the
test and may be held in place by the seated examiner’s thigh. The examiner
grasps the patient’s calf near the popliteal fossa with both hands and attempts
to slide the tibia anteriorly. When the ACL is ruptured, the tibia slides
anteriorly with respect to the femur. The anterior drawer test is performed
several times, with the patient’s foot and leg positioned first in internal
rotation, then in neutral rotation, and finally in external rotation. As in the
Lachman test, the injured knee must be compared with the normal one. The
anterior drawer test is useful for detecting complete ruptures of the ACL but
is often less sensitive than the Lachman test in diagnosing partial injuries.
· Pivot shift and jerk
tests: These tests identify most cases of clinically
significant knee instability. The patient should be lying supine and relaxed,
although this is often difficult in the acutely injured patient because this
test can reproduce a feeling of discomfort. It has been found that this test is
most accurate when performed on an anesthetized patient. The examiner stands
beside the injured leg, facing it. With one hand grasping the patient’s foot,
the examiner places the other hand on the lateral aspect of the knee, with the
thumb underneath the head of the fibula. With the knee starting in full
extension (pivot shift) or flexed to 90 degrees (jerk test), a valgus force is
applied at the knee while the tibia is internally rotated by the hand holding
the foot. This maneuver causes the lateral tibial plateau to subluxate
anteriorly on the femur. With the knee in extension, the iliotibial tract is
anterior to the instantaneous center of rotation of the knee and acts as an
extensor. The knee is then slowly flexed (pivot shift) or extended (jerk test),
and the subluxation becomes more apparent. At a point between 20 and 40 degrees
of flexion, the iliotibial tract slides posterior to the instantaneous center
of rotation of the knee and acts as a flexor, causing reduction of the tibia.
The reduction is palpable, visible, and frequently audible.
 |
| RUPTURE OF CRUCIATE LIGAMENTS: ARTHROSCOPY |
Treatment. Not all acute
injuries of the ACL require surgery. If
the careful physical examination, using anesthesia if necessary, reveals
minimal ligamentous laxity and no sign of meniscus injury and the patient does
not have sensations of instability or symptoms preventing full function, then
prompt, vigorous rehabilitation is instituted. If
the Lachman or anterior drawer test indicates mild ligament instability but the
pivot shift test is negative and there are no other associated injuries, a
nonoperative program may be instituted. However, significant instability may
eventually develop if injury of the ACL is neglected or treated conservatively.
It has been shown that a chronically ACL-deficient knee can also lead to
degenerative tears of the meniscus and eventually an earlier onset of
osteoarthritis. Patients whose knees
give way during daily activities are candidates for delayed reconstruction of
the ligament. If the instability is a problem only during intense physical
activity, using a brace may provide relief.
Physical therapy focuses on rehabilitation of the
quadriceps and hamstring muscles. Although the knee is reasonably stable,
instability may develop gradually, eventually necessitating reconstruction of
the ACL.
Increased instability may lead to meniscus tears.
Surgical
treatment is usually indicated in patients with complete ACL injury,
symptomatic or clinical instability, and a positive pivot shift test. The
procedure used is dictated by the patient’s lifestyle, expectations and other
medical conditions. Older, sedentary patients may need no surgery, whereas
young, active patients should be considered for repair or reconstruction. The
goals of surgery are to restore stability to the knee to permit return to
activity, prolong the survival of the menisci, and delay the development of
osteoarthritis.
Many techniques are used to repair or reconstruct the
ACL, with specific considerations to be taken into account based on each
individual patient. In the skeletally mature patient, the ligament is
traditionally recon-structed using an arthroscopically assisted approach. The
graft choice in younger patients will usually be a hamstrings or bone-patella-bone
autograft, whereas older patients or those with other contraindications to
hamstrings harvest may use allograft tissue. In skeletally immature patients
with open growth plates, there exist multiple modifications to the traditional
reconstruction methods that avoid compromising the tibial, femoral, or both
open physes. Protected weight bearing is allowed immediately, with some
surgeons advocating the use of continuous passive motion machines and braces in
the early postoperative period. Early and consistent physical therapy is
important to achieve optimal results. Patients should avoid participation in
high-demand sports for 6 to 12 months after surgery.
 |
| RUPTURE OF POSTERIOR CRUCIATE LIGAMENT |
RUPTURE OF POSTERIOR CRUCIATE LIGAMENT
The PCL is the chief stabilizer of the knee in full
extension. The most common causes of rupture of this ligament are
hyperextension of the knee and a direct blow to the anterior aspect of the
flexed knee. Severe varus or valgus stress to the knee after injury to the
collateral ligaments can cause rupture of the PCL.
Physical Examination and Special Tests
A knee lacking a functioning PCL may be hyperextended
during examination. The examiner stands at the foot of the supine patient and
simultaneously lifts both feet by the great toes, observing the amount of
extension at each knee. A knee with rupture of a PCL exhibits noticeable
hyperextension and greater joint laxity than its normal counterpart when varus
and valgus stresses are applied
with the knee in full extension.
· Posterior drawer test:
The posterior drawer test is per- formed with the
patient lying supine on an examining table and the knee in 90 degrees of
flexion. The patient’s foot is stabilized by the examiner’s thigh on the table
as for the anterior drawer test. The examiner uses
both hands to push the proximal tibia posteriorly in an effort to displace it
relative to the distal femur. By alternately pushing and pulling the tibia, the
examiner can determine if the ACL is intact and if the proximal tibia is moving
posteriorly. The examiner must recognize the starting point of the drawer test
to determine accurately which of the two cruciate ligaments is injured.
· Posterior sag sign: With the patient supine and relaxed, a pad is placed under the distal
thigh on the affected side; the heel is allowed to rest on the examining table,
and the calf of the leg hangs unsupported. The examiner observes the knee from
the patient’s side. When a rupture of the PCL is present, the proximal tibia
subluxates posteriorly and the anterior surface of the proximal leg appears to sag.
Treatment. Patients who have
high-demand knee and severe instability are candidates for reconstruction of
the PCL. This is routinely accomplished in an arthroscopically assisted fashion
as with the ACL, with surgical options again being individualized to each
patient. As with the ACL, when avulsion of the bony attachment of the PCL
occurs at either end, primary repair of the avulsion fragment may be performed.
If bone-to-bone repair is not possible, many surgeons may elect to treat the
patient without resorting to surgery. Repairs of the PCL have historically been
less successful than those of the ACL, with higher risk of recurrent
instability after surgery and loss of motion. Injury to the posterolateral
corner of the knee capsule must also be considered and addressed when necessary
at the time of surgery to avoid a poor functional result.
After surgery, the knee may be immobilized in
extension for a period of 2 weeks. Vigorous physical therapy is then instituted
while avoiding activities that place a load on the knee when it is flexed past
90 degrees. Achieving full extension may be very difficult and should be a goal
of therapy, although manipulation under anesthesia may eventually be required.
 |
| PHYSICAL EXAMINATION OF THE LEG AND KNEE |
MEDIAL (TIBIAL) COLLATERAL LIGAMENT INJURY
Injury to the taut MCL is often caused by a valgus
force applied to the knee with external tibial rotation. This may occur by a
noncontact twist event or from a blow to the lateral side of the joint. The
patient will initially describe pain on the medial side of the knee and, with a
complete tear, complaints of the knee giving way into valgus.
Physical Examination. Injury to the
MCL is noted with a positive valgus stress test with the knee in 30 degrees of
flexion as compared with the opposite knee. An injured MCL along with disrupted
ACL or PCL will result in more gapping that occurs when the knee is tested in
full extension. Frequently, but not always, a positive anterior drawer sign
results with external rotation of the tibia as the medial tibial condyle
rotates anteriorly.
Imaging. An abduction
stress film may be used to distinguish ligament injury from epiphyseal fracture
in skeletally immature athletes as a fracture opens at a growth plate and a
ligament tear opens at a joint line. This should be done in 30 degrees of knee
flexion. MRI is also useful to help
to diagnose disruptions or edema in the MCL.
Treatment. Grades I and
II sprains are often treated with the RICE (rest, ice, compression, elevation)
protocol, along with use of crutches while weight bearing and physical
rehabilitation. Complete tears, unless present with other associated injuries
or in a high-demand athlete, are rarely surgically repaired. Surgical options include primary repair, allograft
reconstruction, and repair with anchor fixation for avulsion injuries. When
attempting nonoperative treatment, immobilization should be used for a short
period after acute injury with an unstable knee. However, in patients with only
mild instability, rigid immobilization may not be necessary. The patient should begin a rehabilitation program as soon as possible.
 |
| SPRAINS OF KNEE LIGAMENTS |
LATERAL LIGAMENT AND POSTEROLATERAL CORNER INJURIES
Injury to the lateral (fibular) collateral ligament
(LCL) often occurs with a varus force or twisting moment at the knee. Injuries
to this region of the knee may be associated with injuries to the popliteus
tendon, iliotibial band, popliteofemoral ligament, and peroneal nerve.
Posterolateral ligaments are often injured by a hyperextension mechanism,
frequently with a blow to the anteromedial tibia.
Patients will complain of pain present over the
lateral ligament complex. The knee may also give way when twisting, cutting, or
pivoting. In chronic cases, posterolateral corner injury gives a feeling of
giving way into hyperextension when standing, walking, or running backward.
Physical Examination and Special Tests
In acute cases, there may be increased gapping on a
varus stress test at 30 degrees of flexion and a positive posterolateral drawer
sign. Chronic cases often show a positive reverse pivot shift and external
rotation recurvatum test. The dial test will likely present in all cases of
severe posterolateral ligament disruption.
· Dial test: With the patient either prone or supine, the examiner will place an
external rotation force to the knee through the ankle at 30 degrees of knee
flexion. Increased external rotation of 10 to 15 degrees as compared with the
opposite knee indicates an injury to the posterolateral corner. If positive,
the test is repeated at 90 degrees of knee flexion, and increased external
rotation at this point indicates a concurrent PCL injury.
·
External rotation
recurvatum test: With the patient
supine and a stabilizing downward force placed on the femur, the externally
rotated foot is lifted by the great toe. Increased recurvatum or hyperextension
at the knee indicates an injury to the posterolateral corner. The external
rotation recurvatum test may also be apparent on standing, giving an increased
varus appearance to the knee.
Imaging. On plain
radiographs, a “lateral capsular sign” shows avulsion of the midportion of the
lateral capsular ligament with a small fragment of proximal lateral tibia. This
is associated with a high incidence of an ACL tear and indicates anterolateral
instability. The “arcuate sign” shows avulsion of the proximal fibula with the
posterolateral ligament and is also associated with an ACL injury. As with MCL
injuries, stress view radiographs
and MRI may also be used for diagnosis of these injuries.
Treatment. Similar to injuries to the MCL, grade I and II sprains are treated conservatively with the RICE protocol, crutches, and physical rehabilitation. In complete tears, primary surgical repair or allograft reconstruction is usually preferable, especially if the injury involves more than just the LCL. Immobilization alone may be less successful for these injuries in patients with severe instability. Cases of mild instability may be treated onoperatively similar to that for lesser-grade sprains.






























