GESTATIONAL
TROPHOBLASTIC DISEASE
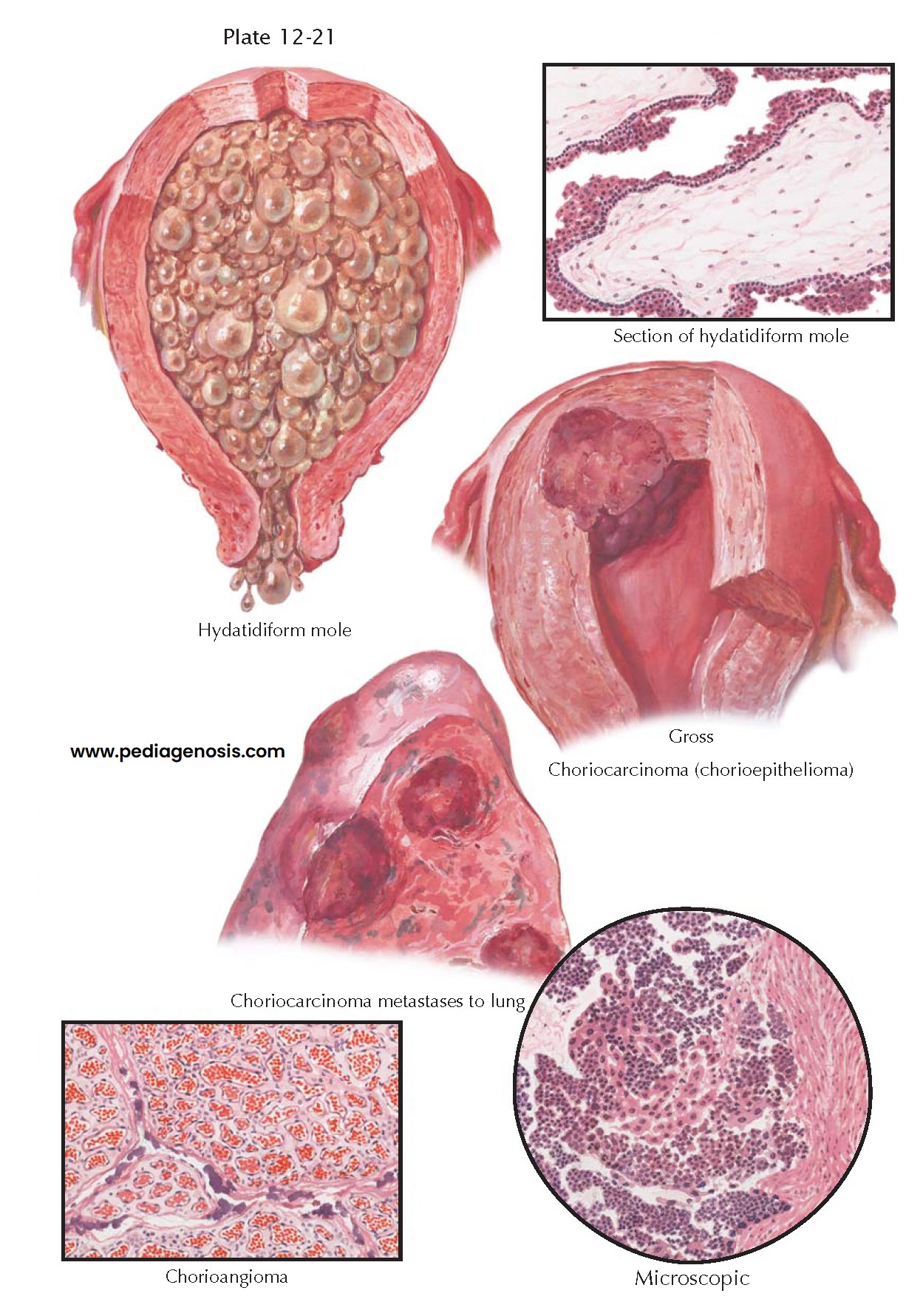
Four neoplasms of placental tissues are known, namely, chorioangioma arising from placental capillaries, hydatidiform mole and choriocarcinoma arising from trophoblastic tissues, and placental-site trophoblastic tumor. Chorioangiomas are rare benign vascular tumors arising from the primitive chorionic mesenchyme, whose etiology is unknown. They are associated with increased maternal age, diabetes mellitus, and hypertension and are more common in multiple pregnancies. The tumor appears as a solitary, deep red, often-lobulated nodule in the placenta. It is of little clinical significance.
A hydatidiform mole
consists of chorionic villi, which appear as grapelike clusters of vesicles.
Moles are classified as being either complete, in which no fetus is present, or
incomplete (partial), in which both fetus (generally abnormal) and molar
tissues are present. The vesicles resemble youthful villi in that they are
branching structures covered with two or more layers of trophoblastic cells,
but they have no fetal blood vessels, and their stroma is only a loose-meshed
matrix filled with clear gelatinous material. Molar pregnancy occurs in 1 of
1000 to 1500 pregnancies in the United States, and as high as 10 per 1000
pregnancies in Asia. Molar pregnancies have the unique genetic attribute of a
double contribution from the father: complete moles are mostly 46,XX all of
paternal origin, though mitochondrial DNA of maternal origin remains;
incomplete moles are most often triploid (69,XXY or 69,XXX) all of paternal
origin.
The clinical
manifestations are the same as those in normal pregnancy, except that the
uterus enlarges more rapidly than usual and there are exaggerated symptoms of
pregnancy. Diagnosis is facilitated by the passage of some grapelike vesicles,
by the abortion of the mole, or a classic “snowstorm” appearance on
ultrasonography. Molar pregnancies are associated with hypertension,
preeclampsia, proteinuria, nausea, and vomiting (hyperemesis, 8%); visual
changes, tachycardia, and shortness of breath are all possible.
(Pregnancy-induced hypertension in the first trimester is virtually diagnostic.)
The treatment of molar
pregnancies is surgical: evacuation of the uterine contents. This is most often
accomplished via suction curettage. Because of the large size of some molar
pregnancies and a tendency toward uterine atony, concomitant oxytocin
administration is advisable and blood for transfusion should be immediately
available. Once the uterus has been emptied, the patient should be closely
followed for at least 1 year for the possibility of recurrent benign or
malignant disease. Any change in the patient’s examination, an increase in β-hCG titers, or a failure of the β-hCG level to fall below 10 mIU/mL by 12 weeks
after evacuation should be evaluated. Serum hCG levels are generally monitored
every 2 weeks until three consecutive tests are negative, then monthly for 6 to
12 months. Pregnancy should be prevented for about a year, because a rising titer in the nonpregnant woman may
indicate the presence of choriocarcinoma.
Gestational trophoblastic neoplasia is notable for the possibility of malignant transformation, although less than 10% of patients develop malignant changes. Choriocarcinoma, also called chorioepithelioma, is a rare but very malignant tumor that metastasizes early to the lungs. It is composed of both syncytial and cytotrophoblastic cells that do not form chorionic villi but grow destructively into the uterine wall. In about half the cases, it follows a hydatidiform mole; in the others, it follows an abortion or a term pregnancy or is, in rare instances, associated with a teratoma. Roughly 80% of molar pregnancies follow a benign course after initial therapy. Between 15% and 25% of patients develop invasive disease, and 3% to 5% eventually have metastatic lesions. The prognosis for patients with primary or recurrent malignant trophoblastic disease is generally good (>90% cure rate). Fewer than 5% of patients will require hysterectomy to achieve a cure for choriocarcinoma.