Elder
Abuse
Elder
abuse refers to the maltreatment and neglect of adults 60 years of age or
older, usually by a caregiver or other person upon whom the elder is dependent.
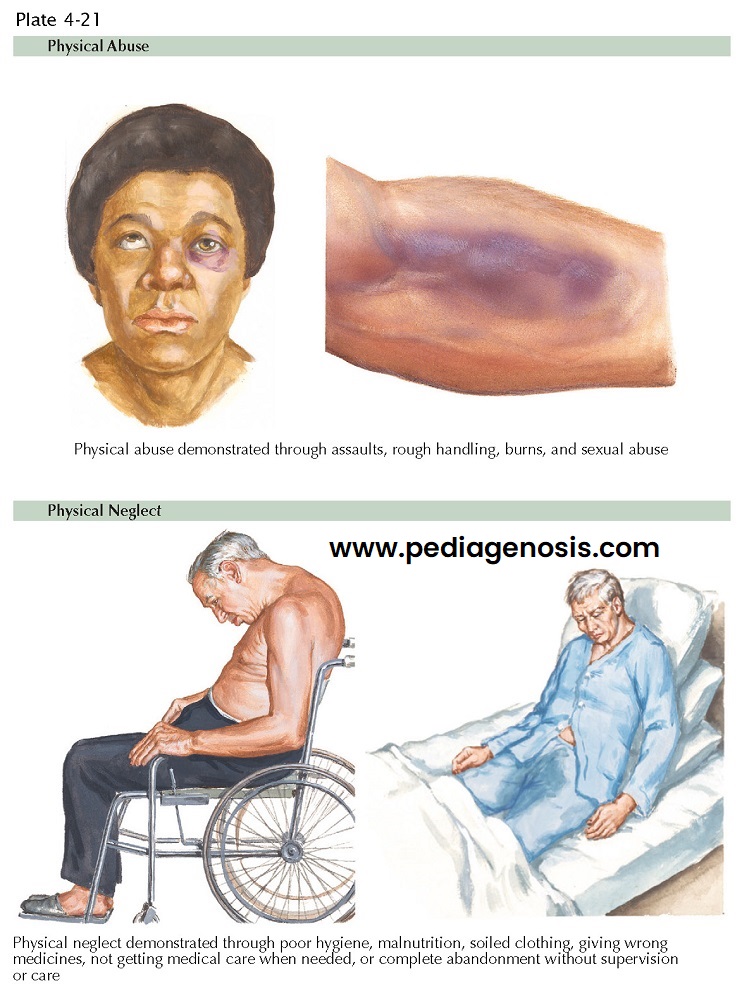
It includes physical abuse (injury, physical threats or inappropriate
restraints), sexual abuse (sex acts or sexual contact without the
elder’s consent), psychologic or emotional abuse, neglect (failure to
meet the elder’s physical, emotional, and social needs or to provide
protection), abandonment, or financial abuse (inappropriate use of the
elder’s resources for personal gain, including forgery, theft, manipulation of
the elder to transfer money or belongings, and exploitation of guardianship or
power of attorney).
According to the National Elder Abuse Incidence Study, in 1996 there were 551,000 documented victims of elder abuse, neglect, or self-neglect in domestic settings in the United States. Only 115,000 (21%) of those victims, however, were fully verified by adult protective services. Thus most cases of elder abuse were either never reported to adult protective services or were ultimately never confirmed by the agencies involved. Victims of elder abuse are often reluctant to report abuse due to fear of losing their caregivers or social supports.
Clinical
Presentation and Diagnosis. Risk factors for perpetrating elder abuse include active mental illness,
alcohol abuse, insufficient training for caregiving, personal history of
physical or emotional abuse, significant emotional or financial dependence upon
the elder, inadequate social support, lack of elder support services, negative
cultural beliefs about elders and aging, and institutional settings with poor
working conditions for staff and/or insufficient administrative monitoring of
elder treatment.
The abused elder
individual must be listened to because he or she often reports the
maltreatment, per se, or there may be abrupt changes in his or her behavior;
sometimes rather unusual behaviors develop. The caregiver may refuse to permit
visitors from seeing the elder alone. However, when observational opportunity
presents, signs and symptoms of elder abuse include bruises, welts,
cuts, lacerations, rope marks or other signs of being restrained, broken bones,
or internal bleeding. In addition, the abused elder patient may evidence injury
to the breasts or genitals, unexplained sexually transmitted illnesses,
dehydration, malnutrition, bed sores, poor hygiene, and unauthorized or
unexplained banking transactions. Laboratory results often indicate medication
overdose or inadequate dosing.
Prevention and
Management. Caregivers
can use a variety of strategies to reduce stress and decrease their own
likelihood of perpetrating elder abuse. First, obtaining adequate training
before assuming elder care responsibilities can markedly reduce feelings of
inadequacy and frustration during caregiving. Caregivers should also enlist the
help of other members of the community, including family, friends, and local
services that have additional resources to assist in caregiving.
Respite for caregivers
between long shifts can significantly decrease stress and is made feasible by
volunteer programs that offer temporary relief from caregiving tasks and
related errands. Adult daycare programs can be highly beneficial. Moreover,
involving independent financial planning services in the management of an elder’s assets can decrease the risk
of financial abuse. Finally, caregivers should never hesitate to seek mental
health counseling for themselves, should they develop feelings of depression or
a substance use disorder.
At elder care facilities,
regular monitoring for abuse, clear policies and protocols outlining proper
elder treatment, thorough employee training, and regular visits to the facility
by community members may all decrease the risk of elder abuse.
Suspected elder abuse
should be reported to adult protective services. The patient may require
hospital admission to ensure safety and provide medical or surgical treatment
in the aftermath of abuse. Attempts should be made to help place the patient in
a safe home, or alternatively, the patient should be allowed to return home if he or she has decision-making
capacity and declines treatment interventions. A multidisciplinary team
approach to elder abuse interventions is optimal and should include physicians,
nurses, social workers, visiting nurses, and caseworkers from adult protective
services.
Course. Victims of elder abuse are at increased risk of adverse health consequences that can differ from the health impact of normal aging, including physical injuries, malnutrition, dehydration, poor sleep, elevated risk of sexually transmitted illnesses, exacerbation of preexisting medical conditions, and premature death. Psychologic sequelae include increased rates of depression, anxiety disorders, symptoms of po ttraumatic stress disorder, and other forms of distress.