DISORDERS OF THE PATELLA
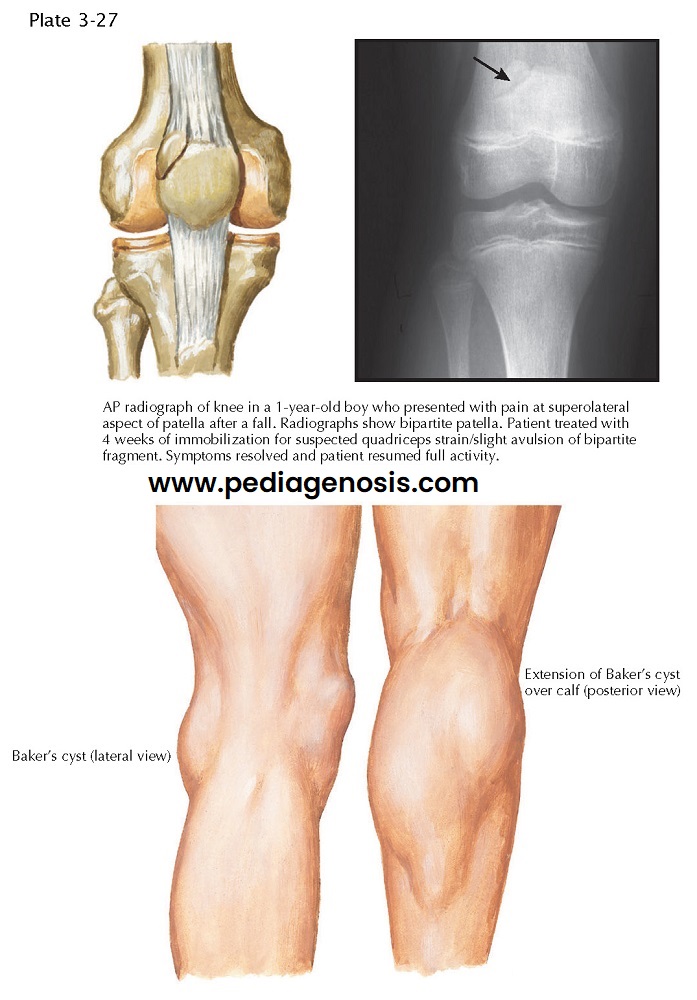 |
| BIPARTITE PATELLA AND BAKER’S CYST |
Congenital fragmentation of the patella is relatively common. One type, bipartite patella, occurs in 1% to 2% of the population. This anatomic variant represents a true synchondrosis (a joint whose surfaces are connected by a cartilaginous plate). Most fragmented patellae remain asymptomatic, but, occasionally, direct trauma to the patella disrupts the synchondroses, causing symptoms that mimic those of a fracture.
A true fracture is differentiated from congenital
bipartite patella on the basis of a history of significant trauma to the
patella, hemarthrosis of the knee, point tenderness over the defect, and a
sharply outlined fragment seen on the radiograph. If the diagnosis is still
uncertain, CT or MRI can be used to differentiate an acute fracture from a congenital
condition.
Asymptomatic bipartite patellae do not require any
treatment. In symptomatic cases, conservative treatment, including a period of
immobilization followed by stretching and strengthening exercises for the
quadriceps and hamstring muscles, is usually sufficient. If the fragment
remains symptomatic, it can be excised along with a lateral retinacular
release.
PATELLA ALTA AND INFERA
Patella alta refers to an abnormally high patella in
relation to the femur. Patella alta predisposes to patellar subluxation and
dislocation with resultant repetitive microtrauma and inflammation of the
patellofemoral joint (patellofemoral chondrosis).
Patella infera indicates an abnormally low patella.
Although it occurs most often secondary to soft tissue contracture and
hypotonia of the quadriceps muscle after surgery or trauma to the knee, it may
also represent a congenital variant.
Imaging. The position
of the patella can best be determined on the lateral radiograph with the knee
flexed 30 degrees. Insall’s ratio describes that the length of the patellar
ligament is usually equal to the diagonal length of the patella. Variations of
more than 20% are considered abnormal.
Treatment. Congenital
patella infera is frequently asymptomatic and requires no treatment. If this
condition develops after injury or surgery, it can be cata- strophic. Prompt
recognition of the condition is of utmost importance because treatment in the
early stages can reverse it. Vigorous rehabilitation of the quadriceps muscles
and mobilization of soft tissue structures around the knee should be instituted
as soon as the complication is recognized.
SUBLUXATION AND DISLOCATION OF PATELLA
The patella depends on both dynamic and static
stabilizers to maintain its proper position in the intercondylar groove.
Although the entire quadriceps muscle contributes to the dynamic stability of
the patella, the contribution of the vastus medialis muscle is critical. The
distal oblique portion of this muscle resists lateral migration of the patella.
The static patellar restraints, which include the bony contour of the distal
femur, the joint capsule, the medial and lateral retinacula, and the medial
patellofemoral ligament (MPFL), are equally important. A flat lateral femoral
condyle (“tabletop” femur) allows the patella to slide laterally quite easily,
whereas a deep intercondylar groove generally keeps the triangular-shaped patella well located. A large Q angle seems to
increase the patient’s susceptibility to subluxation or dislocation of the
patella. The Q angle is formed by the intersection of two lines drawn from the
anterior superior iliac spine and the tibial tuberosity through the center of
the patella. This condition is also often associated with knock-knee and
external tibial torsion and is most commonly symptomatic in adolescent girls
and young women.
Patellar subluxation is the partial
loss of contact between the articular surfaces of the patella and femur. It is
most common when the ligamentous support is loose and when the vastus medialis
muscles are poorly developed or atrophied. Just a weak medial quadriceps muscle permits lateral subluxation, and tightness in
the lateral peripatellar tissues can pull the patella laterally. Patellar
dislocation is the complete loss of contact between the articular surfaces
of the patella and femur. Congenital dislocations are rare and when present
tend to be bilateral and familial. The majority of dislocations are traumatic.
Underdeveloped femoral condyles, insufficient soft tissue restraints, and a
weak vastus medialis muscle all
predispose to patellar dislocation.
Physical Examination. Patients
complain of anterior knee pain, particularly when climbing stairs, and giving
way of the knee. Physical examination reveals tenderness along the medial
aspect of the patella, patellofemoral crepitus, atrophy of the quadriceps
femoris muscle
(especially the oblique portion of the vastus medialis), and increased lateral
mobility of the patella. On physical examination, the patella can normally be
manually displaced both medially and laterally between 25% and 50% of the width
of the patella. Greater movement indicates loose patellar restraints, a finding
frequently seen in adolescent females. A positive apprehension test may be
elicited when the patient forcefully contracts the quadriceps femoris muscle
and feels pain as the examiner attempts to displace the patella laterally. If
the subluxation is not treated, the lateral retinaculum gradually becomes
contracted, exacerbating the abnormal patellofemoral tracking.
Imaging. In addition to
traditional anteroposterior and lateral plain radiographs, it can be beneficial
to obtain an infrapatellar view with the knee flexed 30 to 45 degrees, rather than the traditional “sunrise” or
“skyline” view with the knee flexed beyond 90 degrees. To assess the soft
tissue attachments and stabilizers and bony anatomy the surgeon may choose to
obtain MR images and CT scans, respectively.
Persons at risk for patellar instability may often
exhibit generalized ligamentous laxity and a poorly developed vastus medialis
muscle. When these patients are sitting or standing erect in a relaxed
position, the patellae often face laterally (“owl-eye” patellae). At full
extension, the patella may also deviate laterally outside of the groove (J
sign).
Rupture of the MPFL after lateral dislocation of the
patella causes pain and tenderness along the medial retinaculum. Sometimes, the
vastus medialis muscle is avulsed from the medial intermuscular septum, causing
pain in the medial region of the knee. However, patellar dislocation should not
be confused with a sprain of the MCL. After an acute dislocation of the
patella, gentle manual lateral subluxation of the patella produces dis-comfort, a finding not seen with injury to the MCL.
CHONDROMALACIA PATELLAE
The term chondromalacia describes the softening
and fissuring of the articular hyaline cartilage and frequently refers to the
undersurface of the patella. Chondro-malacia may result from an excessive load
on the patellofemoral joint, but disuse may be a contributing factor.
In clinical practice, chondromalacia is used to describe
inflammation of the articular surface of the patellofemoral joint
(patellofemoral chondrosis) or degeneration of this joint (patellofemoral
arthrosis). Patellofemoral chondrosis is most common in young women.
Contributing factors include weakness and tightness in the quadriceps muscle,
abnormalities of lower limb alignment (knock-knee, bowleg, an abnormally
positioned patella), and obesity. Patellofemoral arthrosis usually occurs with
aging. Patients affected by this will often report pain in the anterior knee
while climbing stairs or sitting for long periods.
Physical Examination. On
examination, compression of the patella may cause pain along the medial and
lateral retinacula and the patellar ligament. Compression of the patella during
flexion and extension of the knee usually elicits crepitation and discomfort;
swelling may also be present. MRI may also reveal chondral changes along the
undersurface of the patella.
Treatment. Strenuous and
pain-provoking activities should be reduced until symptoms subside. Exercises
to stretch and strengthen
the quadriceps muscle, especially the vastus medialis muscle, should be
initiated immediately. In refractory cases, patients may also benefit from
arthroscopic shaving of loose articular fragments or lateral release of the
patella, or both. Although removal of the degenerated tissue usually does
little to alleviate the symptoms or to improve the long-term prognosis, it can
decrease crepitation and synovial effusion. A lateral release may relieve
excess patellofemoral contact pressure or denervate a sensitive region.
 |
| SUBLUXATION AND DISLOCATION OF PATELLA |
PATELLA OVERLOAD SYNDROME
Patella overload syndrome is a common and painful
condition seen in rapidly growing adolescents whose bones appear to be growing faster than the attached soft tissues. This rapid
growth results in tightness of the quadriceps and hamstring muscles, which can
increase the compression forces between the patella and femur during knee
flexion, causing irritation. Trauma can also contribute to the development of
this condition, particularly if followed by immobilization or disuse. These may
lead to soft tissue contracture, resulting in a tight patellofemoral joint.
Patients complain of a toothache-like pain over the anterior surface of the knee, especially along the lateral border of the patella. Conservative management with muscle and soft tissue stretching and strengthening is usually sufficient, but the patella must be protected without further irritation. If exercise causes pain, the routine must be carefully evaluated.




