Child
Abuse
Child
abuse is defined by the Child Abuse Prevention and Treatment Act (CAPTA)
as “Any recent act or failure to act on the part of a parent or caretaker that
results in death, serious physical or emotional harm, sexual abuse or
exploitation; or an act or failure to act that presents an imminent risk of
harm.” There are four major types of maltreatment: neglect, physical abuse,
psychologic mal-treatment, and sexual abuse. Most states set up their own
guidelines indicating the level of evidence to make the distinguishing finding
or disposition for the abuse.
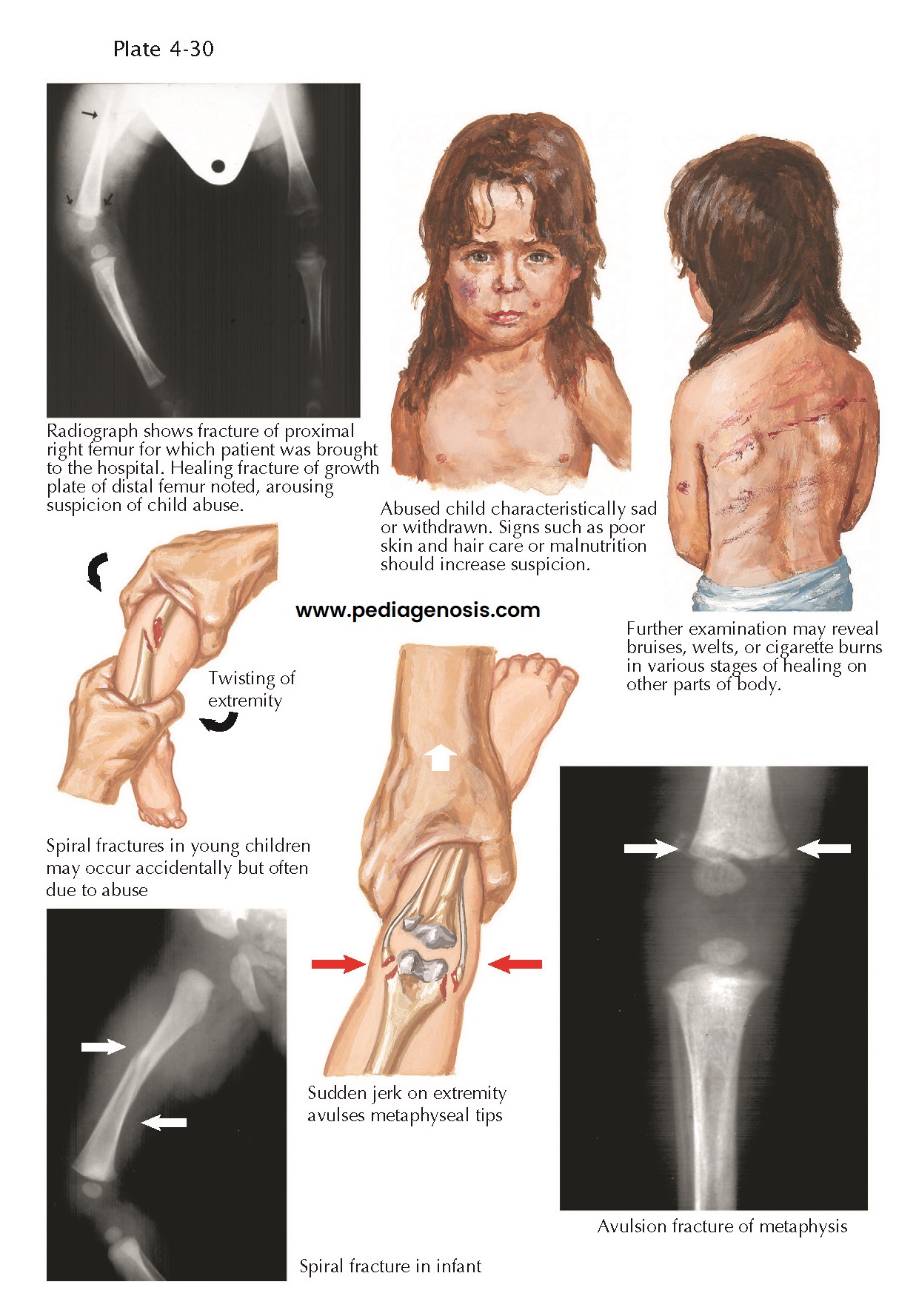 |
| FRACTURES IN ABUSED CHILDREN |
The National Child Abuse and Neglect System (NCANDS) of the Administration of Children, Youth, and Families (ACYF) Annual Report 2009 indicates that there were 9.3 unique abuse victims confirmed per 1,000 children in the United States. Children 1 year and younger had the highest rate of victimization; there was an almost equal distribution of boys and girls; some children experienced multiple abuses. Neglect was most frequent (78.3%), followed by physical abuse (17.8%). Sexual and psychologic maltreatment each occurred in 10% of abused children overall. The 2009 national fatality rate was 2.34 per 100,000 and has been increasing over the past 5 years. Health and mental health-care professionals should maintain the possibility of abuse on their differential every time they see a child.
Clinical
Presentation. Presentations
vary greatly depending on the type(s) of abuse as well as social and emotional
developmental stage. Children with developmental disabilities, that is, mental
retardation, emotional disturbances, visual or hearing impairment, learning
disabilities, physical disabilities, behavior problems, or other medical
problems are at increased risk
of being victims.
Physical abuse most often manifests with signs of
abuse, including bruising and/or skeletal injury. In addition, physical
abuse is often associated with psychologic impacts, including increased anger,
aggression, poor academic performance, sleep problems, drug abuse, and
suicidality. Sexually abused children often present to physicians for
evaluation of genital injury. The sequelae includes impaired mental
health with increase in rates of depression, anxiety disorders, sleep
disorders, suicide attempts, and posttraumatic disorder (PTSD), but not schizophrenia or somatoform
disorders.
With psychologic
abuse, it is more
difficult to quantify and identify consistent patterns of presentation.
Children of psychologic abuse present with increased levels of depression,
academic difficulties, aggression, and behavior problems. Often, children are exposed to more
than one type of abuse, and so the impact of abuse can be complex. In addition,
physical, sexual, and psychologic abuse are associated with poor self-esteem, personality disorders,
and impaired interpersonal relationships.
Diagnosis. Evaluations must be carried out by
qualified pediatric health-care professionals, such as child and adolescent
psychiatrists, pediatricians, child psychologists, child-trained social
workers, pediatric counselors, and clinical nurse specialists, depending on the
type of abuse—physical and/or psychologic. If there is a concern about physical
abuse, physical and diagnostic examinations should be performed as soon as
abuse is suspected. With concern about sexual abuse, pregnancy tests and/or
sexually transmitted infections must be evaluated. In all instances,
information should be gathered from multiple people within the child’s
psychosocial sphere (e.g., parents/caregivers, family members, teachers,
counselors).
Treatment. The first step after identification
of suspected abuse is reporting to a child protective service (CPS) agency. The
CPS will carry out a thorough investigation of the suspected person(s) abusing
the child and their living situation. The CPS will engage a treatment team to
support the child and his or her family. In instances where the child’s safety
has been compromised and/or future abuse is suspected without intervention,
then the child may be placed in a safe environment until the investigation is
complete or sufficient supports are put in place for the child to return home.
The primary treatment for child abuse includes psychotherapy, which can include
components of cognitive-behavioral therapy (change behavior by addressing
distorted cognitions), behavioral and learning therapy (modifying habitual
responses to situations/ stimuli), family therapy (explore patterns of family interactions), and developmental
victimology (describes the processes involved in the onset and maintenance of
abusive behavior).
Course. Child abuse is hypothesized to mediate response biases, resulting in impaired emotional and cognitive regulation. Adult victims of prior childhood abuse are found to have higher rates of sleep disorders, abdominal disorders, obesity, chronic pain (e.g., head-ache, back ache, premenstrual syndrome), fatigue, and exaggerated startle responses. Longitudinal studies indicate that adults continue to suffer from low self-esteem, maladaptive sexual behavior, and impaired interpersonal relationships (e.g., parenting, romantic/ intimate). Despite these findings, not every child who experiences abuse develops these symptoms, indicating a role for protective factors, such as cognitive factors, meaningful relationships, and the impact of treatment interventions.































