INFECTIONS
Infections of the ovaries are usually secondary, with most the result of cervical gonococcal or chlamydial infections that have ascended into the upper genital tract (pelvic inflammatory disease [PID]). Tubercular infections and infections in the gastrointestinal tract (particularly in association with appendicitis) also occur. Transmission may be through direct contact with infections of contiguous organs; lymphatic spread, particularly of streptococcal infections of the uterus to the ovarian hilum; and hematogenous extension from distant foci, as may occur in mumps, scarlatina, measles, diphtheria, tonsillitis, typhoid fever, and cholera.
Acute oophoritis due to surface invasion may be mild and superficial,
resulting in thin, fibrinous periovarian adhesions. Chronic perioophoritis is
evidenced in the residuals of PID, where dense, fibrous adhesions bind the ovary
to the tube, posterior surface of the broad ligament, and lateral pelvic wall.
Microscopically, a diffuse oophoritis may show hyperemia, edema, and leukocytic
infiltration. The presence of multiple small abscesses indicates a lymphatic
invasion. The open punctum of a ruptured graafian follicle or a thinly covered
current hemorrhagic corpus luteum offers a favorable point of entry for
contiguous infection. At times, an expanding ovarian abscess may replace the
entire ovary. Fusion with the tube, or pyosalpinx, fol- lowed by a breakdown of
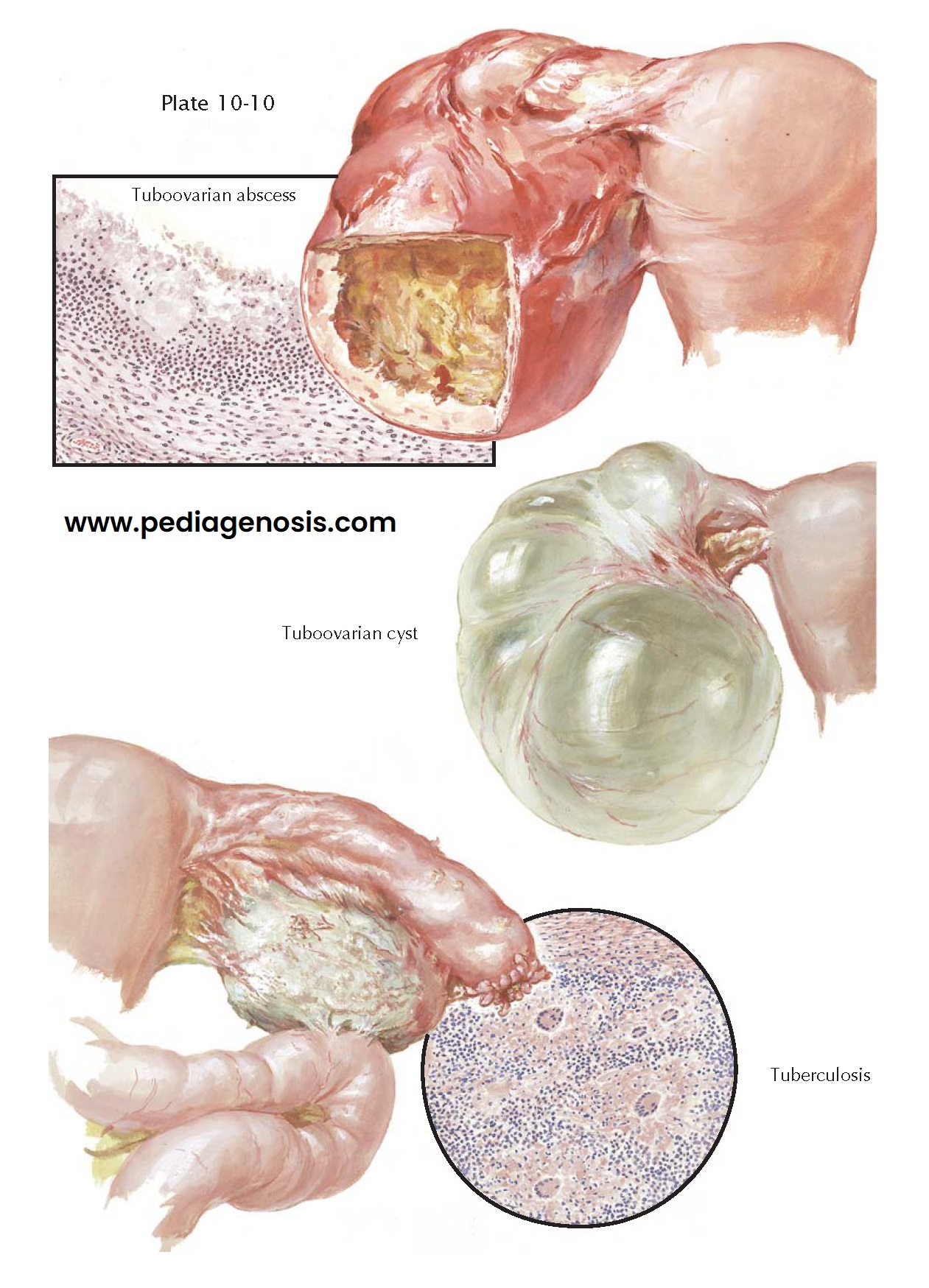
intervening tissue, results in a tuboovarian abscess.
Streptococci and colon bacilli may secondarily infect a tuboovarian
abscess of gonorrheal origin. Clinically, it is indistinguishable from a large
pyosalpinx. Tubo-ovarian abscesses may gradually resolve, exacerbate
intermittently, perforate locally to form a large pelvic abscess, or rupture
into the rectum, bladder, vagina, or abdominal cavity. A chronic tuboovarian
abscess may be relatively quiescent or asymptomatic. In the more acute state,
it may give rise to low abdominal pain, nausea, vomiting, abdominal distension,
evidences of pressure upon the bladder and rectum, fever, lower abdominal spasm
and tenderness, leukocytosis, and a rapid sedimentation rate. Pelvic
examination may reveal a fixed retrodisplaced uterus and bilateral, soft,
irregular, fixed, tender masses laterally and behind the uterus. With subsidence
of the infection and resorption, a tuboovarian cyst may result. These are
large, retort-shaped, thin-walled, cystic structures, densely adherent to the
pelvic peritoneum, broad ligament, and uterus. Tuboovarian abscesses must be
differentiated from ovarian neoplasms with infarction, secondary infection, or
rupture; appendicitis with pelvic abscess; diverticuli- tis; ovarian, tubal, or
sigmoidal carcinoma; endometrio- sis; and ruptured tubal pregnancy with
hematocele.
Streptococcal infections of the ovary and contiguous structures may
follow postoperative or puerperal infections, instrumentation or cauterization
of the cervix, insertion of a radium “tandem,” and cervical stenosis with
pyometra. Parametritis and pelvic cellulitis may progress until a firm, brawny,
fixed, tender mass fills the posterior cul-de-sac and extends across the pelvis
to the lateral pelvic walls. The ovaries are secondarily involved by lymphatic
spread and contact. Large abscesses may be formed that may be drained, may
perforate, resolve, and recur.
Pelvic tuberculosis is almost invariably secondary to an old or recent acid-fast infection elsewhere, particularly of the lungs. The hematogenous route first involves the tubal endosalpinx, usually bilaterally, followed by direct invasion of the myosalpinx, perisalpinx, and pelvic peritoneum. This is often followed by perioophoritis, with penetration into the ovarian cortex. Thus, tuberculosis of the ovary is secondary to a tuberculous salpingitis by contiguity. The ovary may appear grossly normal or slightly enlarged, studded with tubercles and covered by dense adhesions. In advanced cases caseation and an ovarian abscess with thick, ragged walls may be seen, sometimes eventuating into a pelvic abscess. Microscopically, only a few tubercles or marked infiltration with caseation may be noted. If resolution does not occur with standard tuberculosis antibiosis, total hysterectomy and bilateral salpingo-oophorectomy offers the best chance for cure.