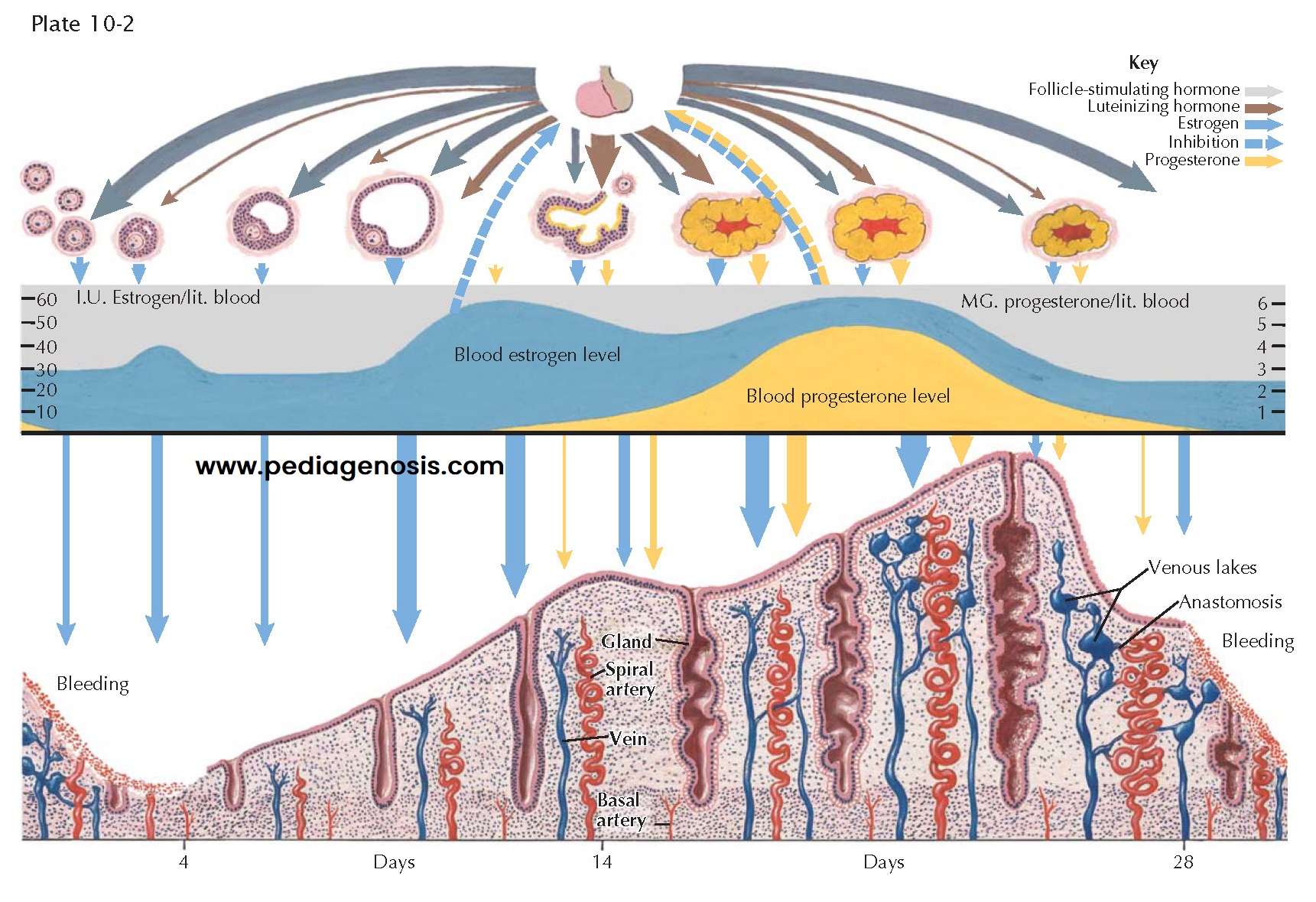
ENDOCRINE RELATIONS DURING CYCLE
Menarche, or the
first menstrual cycle, heralds the onset of adult reproductive function, which
continues until menopause, when the major part of ovarian function ceases.
Between these events, the hormonal ballet of cyclic menstruation takes place.
Two anterior pituitary gonadotropins and two ovarian steroids are primarily involved in this periodic occurrence of menstruation: the pituitary contributes follicle-stimulating hormone (FSH) and luteinizing hormone (LH), whereas the ovary secretes-estradiol and progesterone.
Up to puberty—even during fetal life—ovarian follicles are constantly
developing to a stage in which an antrum has formed, regressing then to become
atretic. Eventually, one or more follicles produce enough estrogen to cause a
proliferation of the endometrium. It is unlikely that any of these early
follicles, though producing estrogen, achieve ovulation; more likely, atresia
sets in and the endometrium breaks down, with resultant bleeding. It is
probable that the mature cycle will not become established for several months
after this, the first menstruation.
At the onset of menstrual flow (day 1), production of estrogen is low but
FSH levels rise and initiate another round of folliculogenesis. A cohort
consisting of a number of follicles begins the maturation process approximately
375 days prior to day 1 of the menstrual cycle. By the onset of menses, these
have matured enough to respond with growth and an increase in estrogen. Most of
the follicles, however, have a relatively short life. Their granulosa cells and
ovum degenerate, leaving an atretic follicle. A few continue to enlarge, but in
most cycles only one emerges as the mature graafian follicle that ruptures or
ovulates about day 14.
Through about day 12 of the cycle, the secretion of FSH decreases with
the increase of estrogen production. Although follicle growth beyond the stage
of antrum formation must be initiated by the pituitary and continues to be
dependent on this stimulus for the first week or so of the cycle, after about
day 8 further development is autonomous. A surge of LH (and to a lesser extent
FSH) at midcycle reflects this rising estrogenic tide and it provides the
endocrine trigger for ovulation.
After ovulation the estrogen level drops slightly during a lag period
between the functional peak of the mature follicle and that of the fully
developed corpus luteum. Some uterine spotting or even bleeding for a day or
two is not rare at this time (“midcycle bleeding”).
Within a few hours after ovulation, the empty cavity of the ruptured
follicle becomes filled with blood clots, and a network of capillary fingers
stretches tentatively inward along fibrin strands from the theca interna. Theca
cells containing a yellow lipochrome, named lutein, proliferate centripetally
at a rapid rate along with the capillary mesh. Progesterone production is
quickly accelerated, and its effect can be detected by secretory changes in the
endometrium within 48 hours after ovulation.
Stimulation of the thermal center in the brainstem, by progesterone,
causes a rise in basal body temperature, which is sustained as long as the
corpus luteum functions. Cervical mucus becomes scanty and viscid and, when
rapidly dried on a slide, no longer crystallizes in a “fernlike” pattern. By
day 20, the estrogen level is usually as high as that just before ovulation,
and the corpus luteum has also reached a peak of production of progesterone.
Under the influence of estrogen and progesterone, growth and the secretory activity of the endometrium progress continuously through day 25 or 26. Unless fertilization has occurred, degeneration of the corpus luteum is initiated. With the consequent decline of both estrogen and progesterone, changes occur in the endo- metrium that lead inevitably to slough and necrosis. By day 28, the pituitary, now released from the inhibitive levels of estrogen, starts again and rapidly reaches its peak of FSH output, which supports a new crop of primary follicles for the next cycle.