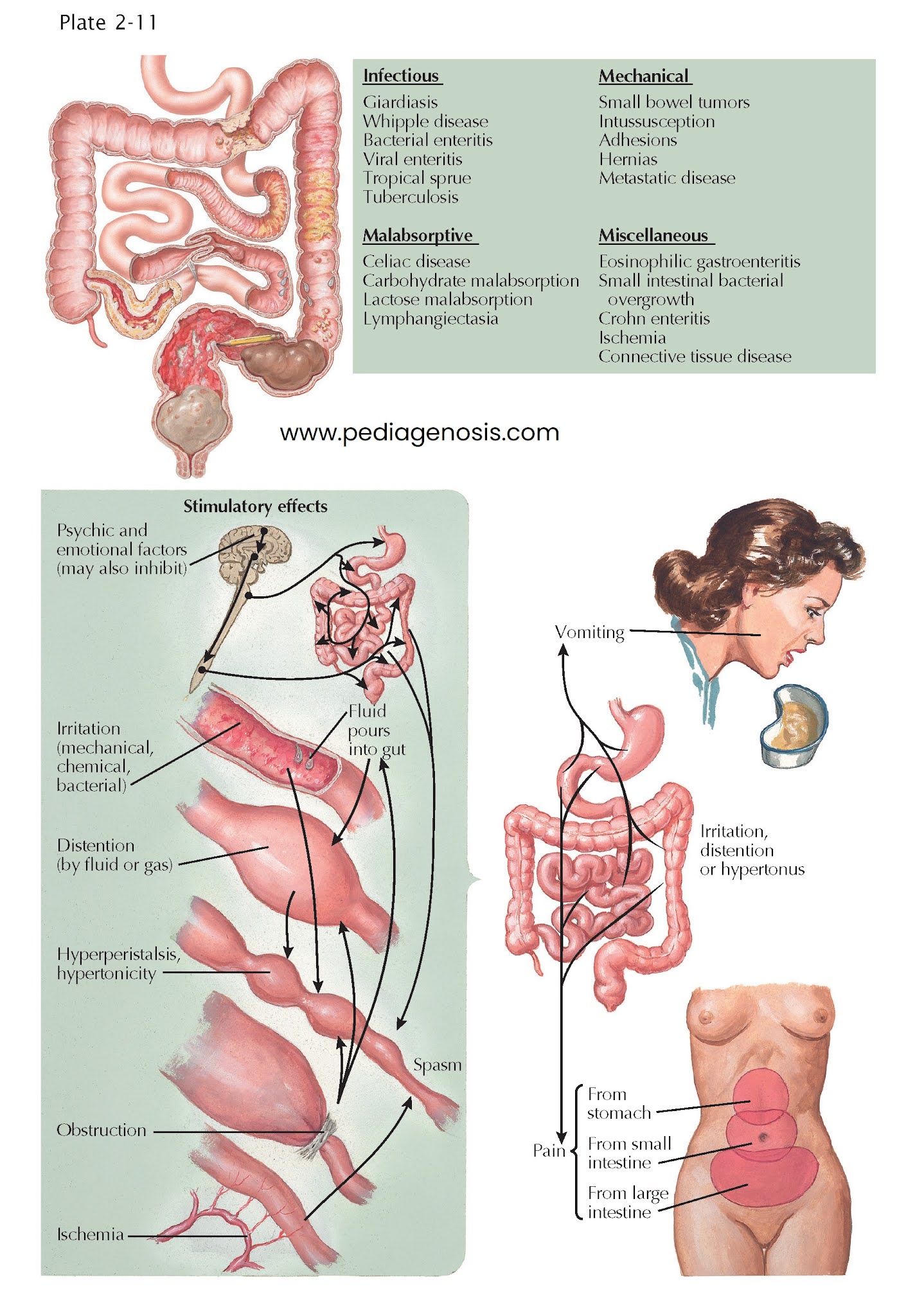
Pathophysiology of Small
Intestine
The most important functions of
the small intestine are digestion and absorption of nutrients. They are
achieved by an interaction between intact small bowel motility and
gastrointestinal hormones. Clinically recognizable disturbances of small bowel
function arise mainly from alterations in the motor activities or interference
with digestion and absorption.
Abdominal pain is a common manifestation of several processes involving the small intestine. The pain is often located in the mid abdomen (periumbilical region) but can also be diffuse across the abdomen. Progressive small bowel distention with or without obstruction causes colicky pain in the early stages, which later becomes constant and unrelenting. Invasive bacteria such as Yersinia can invade the terminal ileum, causing severe pain and tenderness mimicking acute appendicitis. Severe postprandial pain that incites fear of eating (sitophobia) is diagnostic of mesenteric ischemia, especially when it is accompanied by weight loss in an atherosclerotic patient. Crohn disease frequently involves the distal small bowel, with deep transmural ulceration and crampy abdominal pain in the right lower quadrant.
Distention
or irritation of the small bowel tends to provoke nausea and vomiting. The
second portion of the duodenum is so sensitive in this respect that it has been
termed the “organ of nausea.” Small intestinal obstruction from any source
invariably causes vomiting. Luminal blockage by tumors, intussusception,
strictures from Crohn disease, adhesions or other complications of irradiation
or extrinsic processes, internal herniation, or impingement by vascular
structures (e.g., superior mesenteric artery) all present with varying degrees
of vomiting. Enteric infections with viruses such as norovirus or bacteria such
as Staphylococcus aureus often cause vomiting, by elaborating
enterotoxins that cause visceral irritation and induction of ileus.
Acute
profuse watery diarrhea is often infectious in etiology and resolves within 3
to 4 weeks. Chronic diarrhea that lasts more than 4 weeks has a broad
differential diagnosis and includes secretory causes such as ingestion of drugs or toxins,
neuroendocrine tumors, and bile acid malabsorption (choleric diarrhea).
Diarrhea accompanied by weight loss is common in bowel resection or mucosal
diseases such as inflammatory bowel disease (Crohn ileitis), celiac disease
(gluten-sensitive enteropathy), and abetalipoproteinemia. Infectious diseases
can also target the small bowel, as in Whipple disease, Myco acterium
avium-intracellulare infection, and
giardiasis.
DYSMOTILITY
Disordered
small bowel motility, or dysmotility, may be idiopathic, inherited as a
familial visceral myopathy or neuropathy, result from systemic disease or
infection, or occur as a paraneoplastic consequence of malignancy. Mild forms
of intestinal dysmotility may be asymptomatic; symptomatic disease can range
from mild discomfort to bowel obstruction.
BLOATING
Bloating is a sensation of abdominal fullness and is often attributed by patients to excessive gas in the intestine. It can be a sign of intolerance to lactose or of the presence of small intestinal bacterial overgrowth; however, many patients with bloating often have no clearly identifiable abnormality.