Diaphragmatic Hernia
 |
| SITES OF DIAPHRAGMATIC HERNIAS AND HERNIATION OF ABDOMINAL VISCERA |
Diaphragmatic hernia in the newborn is a not uncommon defect and seems to be reported increasingly, in one to four neonates per 10,000 births. This probably reflects earlier diagnosis and more prompt treatment rather than increased incidence. If the diaphragmatic defect is not surgically repaired, most of these infants die within the first month of life as a result of respiratory compromise.
The
most usual site of a congenital diaphragmatic hernia is the foramen of Bochdalek
in the posterolateral portion. Herniation most often occurs in the left side
and usually involves the stomach and the bowels. Right-sided hernias are rare
and may contain the liver. Less common hernias occur at the esophageal hiatus
and at the foramen of Morgagni in the retrosternal portion of the diaphragm.
Herniation through these latter defects usually does not produce severe
respiratory distress. Diaphragmatic eventration must be distinguished
from diaphragmatic herniation. The former refers to elevation of a portion of
the diaphragm that is thin and membranous due to incomplete muscularization.
The diaphragm in this case forms a sac that covers abdominal contents that are
displaced into the thorax. In rare cases, the diaphragm may completely or
partially fail to develop (diaphragmatic or hemidiaphragmatic
agenesis). The cause of congenital diaphragmatic hernia has not been
clearly elucidated; most occur sporadically. Failure of normal closure of the
pleuroperitoneal folds during the fourth to tenth weeks following fertilization
appears to be the initial step in formation of these hernias; genetic or
environmental factors are believed to trigger disruption of mesenchymal cell
differentiation during formation of the diaphragm, however.
Most
cases of congenital diaphragmatic hernia are diagnosed prenatally on routine
ultrasound screening at approximately 24 weeks of gestation. Visualization of a
chest mass with or without mediastinal shift is suggestive of a diaphragmatic
hernia. Fetal MRI can confirm the finding and estimate lung volumes, as well as
identify associated anomalies, which frequently occur with diaphragmatic
hernias. Fetal genetic studies should also be performed. In utero therapy is
investigational at this time and involves fetal tracheal occlusion, which
averts pulmonary hypoplasia and pulmonary hypertension by
increasing transpulmonic pressure. The birth should take place at a tertiary
care center via vaginal delivery induced at term.
Although
routine prenatal ultrasound examination is able to identify most congenital
diaphragmatic hernias, the diagnosis may not be made until after delivery. The
characteristic signs include a barrel-shaped chest with a left-sided
respiratory lag (if the hernia is on the left, as it is in
most instances) and a small and frequently scaphoid abdomen. The heart is
displaced to the right, often to an extreme degree. Breathing sounds are absent
over the left chest and are heard only over the upper right thorax portion,
where they are harsh in character. Gas fills the herniated bowel usually only
later, so that the percussion sounds over the chest are not necessarily
tympanitic directly after birth. Auscultatory findings, suggestive of
peristaltic movements in the chest, may be present but
are not reliable. Some infants, able to compensate for the presence of
abdominal viscera in the chest, exhibit signs and symptoms only when the
gas-filled intestines cause a greater mediastinal shift. Though the diagnosis
can be made on physical findings alone, chest x-ray confirms the clinical
impression, except when the severity of the infant’s respiratory dis- tress
does not allow time for such a procedure.
Once
the diagnosis of a diaphragmatic hernia is made, the management encompasses
preoperative medical management followed by surgical repair. Aggressive
preoperative medical management has improved survival rates to well over 90%
and involves ventilatory support after immediate endotracheal intubation. Use
of extracorporeal membrane oxygenation is reserved for infants who fail to
respond to conventional ventilatory support. Echocardiography is performed to
evaluate pulmonary hypertension and identify underlying cardiac anomalies. The
circulatory system is maintained by administration of fluids and inotropic
agents. To avoid additional distention of the abdominal viscera, nasogastric
tube placement before anesthesia is recommended. Premature infants with
respiratory distress syndrome should receive surfactant therapy.
In
the past, surgical repair of these types of hernias was considered an emergency
and infants underwent surgery shortly after birth. It is now accepted that
emergent surgery is not necessary, and the timing of surgical repair depends on
the severity of pulmonary hypoplasia and pulmonary hypertension. Infants requiring
minimal support with no evidence of pulmonary compromise can undergo surgical
repair within 72 hours. In infants with some degree of pulmonary hypoplasia and
reversible pulmonary hypertension, surgery should be delayed until pulmonary
compliance improves and pulmonary hypertension is reversed.
 |
| THORACIC APPROACH TO REPAIR OF DIAPHRAGMATIC HERNIA |
Surgical
repair of the diaphragmatic hernia can be performed using an abdominal or a
transthoracic approach via either open or minimally invasive techniques.
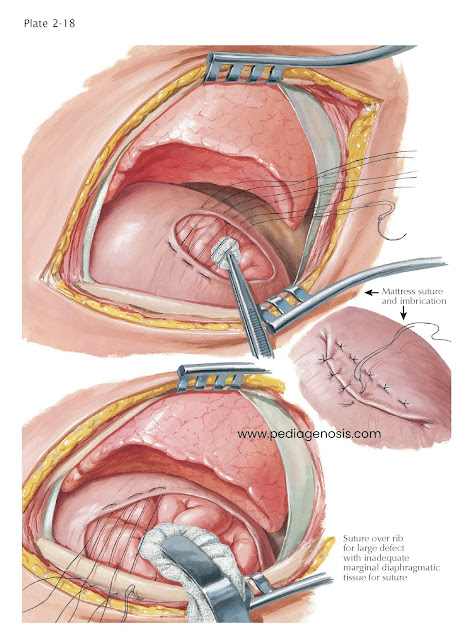
The
repair of the diaphragmatic defect may be accomplished by primary closure;
however, larger defects often need a synthetic patch repair to allow a
tension-free closure. The abdominal cavity may also be too small and
underdeveloped to accommodate the intestine and permit closure of the abdominal
wall muscle and fascial layers. In such cases, a temporary abdominal wall silo
or mobilization of abdominal wall skin flaps may be necessary
to allow for gradual visceral reduction and concomitant abdominal cavity
expansion, so that a staged closure of the abdominal wall is possible.
Complications following repair can be seen immediately after surgery with persistent pulmonary hypertension or can occur late with chronic respiratory disease, recurrent hernia, patch infection, spinal or chest wall abnormalities, and gastroesophageal reflux.




