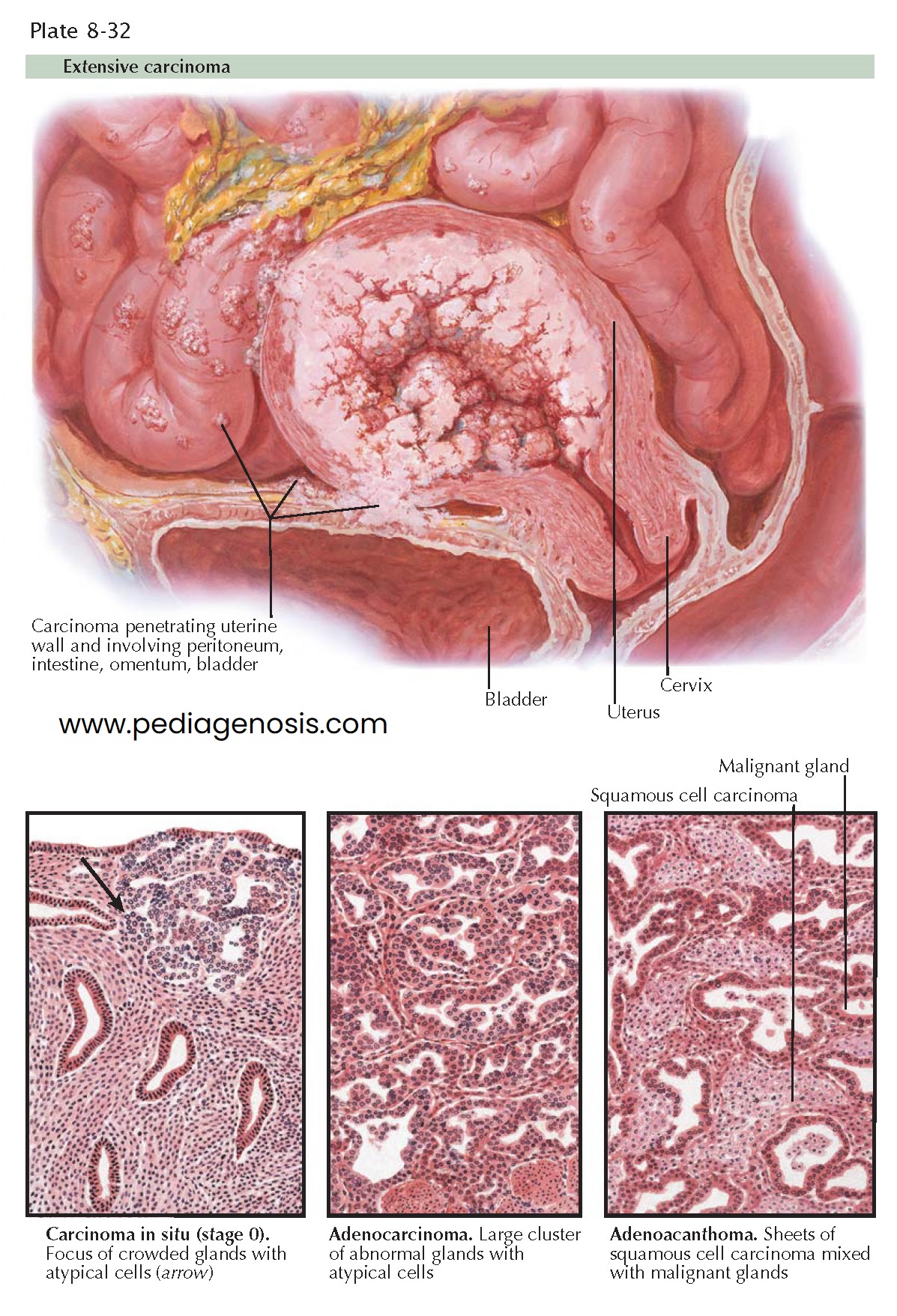
CANCER OF CORPUS II—HISTOLOGY AND EXTENSION
Squamous epithelium commonly coexists with the glandular elements of endometrial
carcinoma. Historically, the term adenoacanthoma was used to describe a
well-differentiated tumor and adenosquamous carcinoma to describe a more
anaplastic carcinoma with squamous elements. The term adenocarcinoma with squamous
elements is now used with a description of the degree of differentiation of
both the glandular and squamous components. Uterine papillary serous carcinomas
are a highly virulent histologic subtype of endometrial carcinomas (5% to 10% of
cases). These tumors histologically resemble papillary serous carcinoma elsewhere
in the body (e.g., ovary). Clear-cell carcinomas of the endometrium are less common
(<5%), and histologi-cally they are similar to clear-cell adenocarcinomas of
the ovary, cervix, and vagina. Clear-cell tumors tend to develop in postmenopausal
women and carry a worse prognosis. Survival rates of 39% to 55% have been reported,
versus 65% or better for endometrial carcinoma.
Successful therapy primarily depends on the surgical extirpation of the disease
while it is confined to the uterus. Unfortunately, many of these patients are not
good surgical risks owing to chronic or intercurrent afflictions common to the sixth
and seventh decades of life. Primary treatment consists of surgical exploration
with hysterectomy, bilateral salpingo-oophorectomy, cytologic examination of the
abdomen and diaphragm, and paraaortic node sampling. For patients with signifi-
cant medical comorbidities, radiation therapy alone can be used, though at a cost
in efficacy. Postoperative radiation to the vaginal cuff reduces local recurrence.
Distant metastatic disease is treated with high-dose progestins, cisplatin, and
doxorubicin (Adriamycin). The use of adjuvant radiation therapy in women with
disease limited to the uterus based on systematic surgical staging is controversial.
For patients with stage I, grade 1 tumors, postoperative radiation (vaginal brachy-
therapy and/or external beam irradiation) may be considered if there is deep myometrial
invasion to the outer one-third or if there is any invasion and the surgical
staging was limited.
The treatment of stage II disease is less well defined. Three therapeutic options
have been employed: primary operation (radical hysterectomy and pelvic node dissection),
primary radiation (intrauterine and vaginal implant and external irradiation) followed
by an operation (extrafascial hysterectomy), and simple hysterectomy followed by
external beam irradiation. Most patients with stage II disease are treated with
a combination of radiation and extrafascial hysterectomy, resulting in 5-year survival
rates that approach 75%.
Patients with stage III and IV endometrial cancer have a high risk of hematogenous
and lymphatic spread of their cancer outside of the pelvis. Therefore, systemic
therapy plays a key role in the management of these patients. Both hormonal and
cytotoxic agents have activity in patients with advanced endometrial cancer. In
addition, there continues to be a role for radiation therapy to gain local control
or to treat pelvic disease. Following treatment, patients should be monitored
by follow-up Pap smears from the vaginal cuff every 3 months for 2 years, then every
6 months for 3 years, and then yearly. A chest radiograph should be obtained
annually. Ten percent of recurrences will occur more than 5 years after initial
diagnosis.
Death results from distant metastases to vital organs more commonly in endometrial carcinoma than in cervical neoplasms. These distant metastases are unquestionably bloodborne. Local obstruction of the ureters is rare.