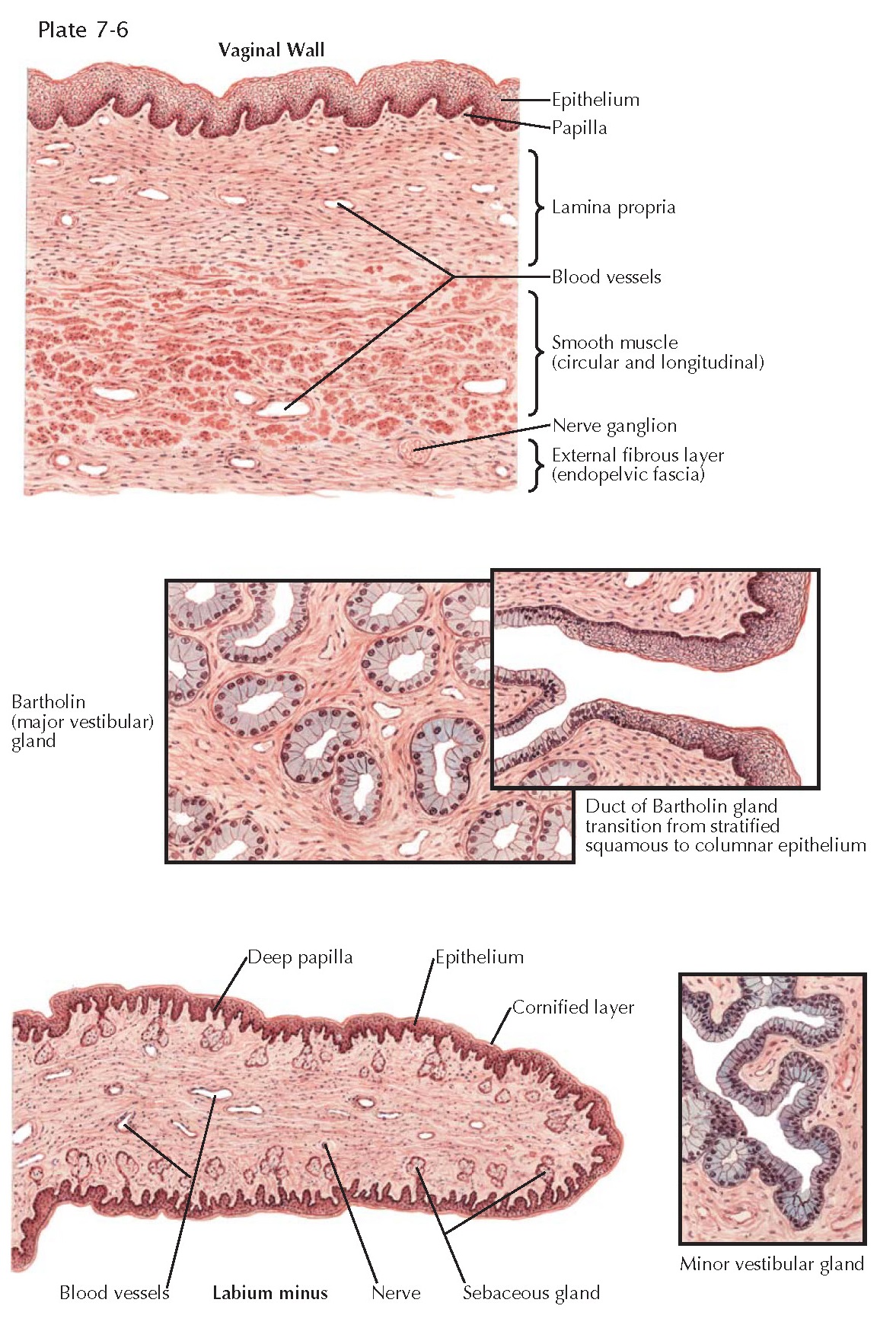
VULVA AND VAGINA HISTOLOGY
The vagina is lined by squamous epithelium and capable of dilation and constriction as a result of the action of its supporting muscles and erectile tissue. The three principal layers are easily recognized in the cross section through the vaginal wall. The epithelial surface is composed of stratified squamous epithelium divided into basal cell, transitional cell, and spinal or prickle cell layers, also referred to as basalis, intraepithelial, and functionalis. The superficial cells contain keratin but normally show no gross cornification in women of reproductive age. The epithelium is slightly thicker than the corresponding structure in the cervix and sends more and larger papillae into the underlying connective tissue, giving the basement membrane an undulating outline. These papillae are more numerous on the posterior wall and near the vaginal orifice. Beneath the epithelium, which has a thickness of 150 to 200 m, a dense connective tissue layer known as the lamina propria is supported by elastic fibers crossing from the epithelium to the underlying muscle. These elastic fibers, here and throughout the pelvis, are critical to pelvic support and function. The lamina propria becomes less dense as it approaches the muscle, and in this area it contains a network of large, thin-walled veins, giving it the appearance of erectile tissue. The smooth muscle beneath this layer is divided into internal circular and external longitudinal groups, the latter being thicker and stronger and continuous with the superficial muscle bundles of the uterus. No dividing membrane or fascia separates these two interlacing muscle groups. The adventitial coat of the vagina is a thin, firm, fibrous layer arising from the visceral or endopelvic fascia. In this fascia and in the connective tissue between it and the muscle runs another large network of veins and, in addition, a rich nerve supply. The Bartholin gland is situated just lateral to the vaginal vestibule and appears in cross section as a collection of small mucus-secreting glands lined by a single layer of columnar epithelial cells with basally placed nuclei. Occasionally, the columnar epithelium is stratified. The small glands tend to be oval and symmetric and are supported in a loose, vascular connective tissue. The main Bartholin duct is lined by columnar epithelium as it runs upward along the side of the vagina, but as it nears its opening in the midportion of the lateral wall of the vestibule, the epithelium takes on the stratified squamous characteristics of the vaginal epithelium. This transition accounts for the fact that malignant tumors of Bartholin gland may be of either the adenomatous or the squamous type.
The minor vestibular glands, situated around the clitoris and urethra and
aiding in the lubrication of the vaginal surface, are of a more racemose,
branching type than Bartholin glands. The
mucus-secreting epithelium of these glands is tall, columnar, and one or two
cells deep.
The labium minus has an epithelium more deeply pigmented than that of the
vagina. The superficial cells are more markedly keratinized and form a horny
(cornified) layer, which is especially prominent in post-menopausal women. The
papillae of the lamina propria push deeply into the overlying epithelium, but
the surface layer is clearly demarcated from the
underlying layers by its basement membrane and often by a thin area of edema.
Close to the surface are located numerous small sebaceous glands but no hair
follicles or fat cells, in contrast to the labia majora. The connective tissue
supporting the labium is acellular but rich in nerves and small vessels. The
veins are not so numerous or so large as thos in the vagina and cannot be
regarded as erectile tissue.