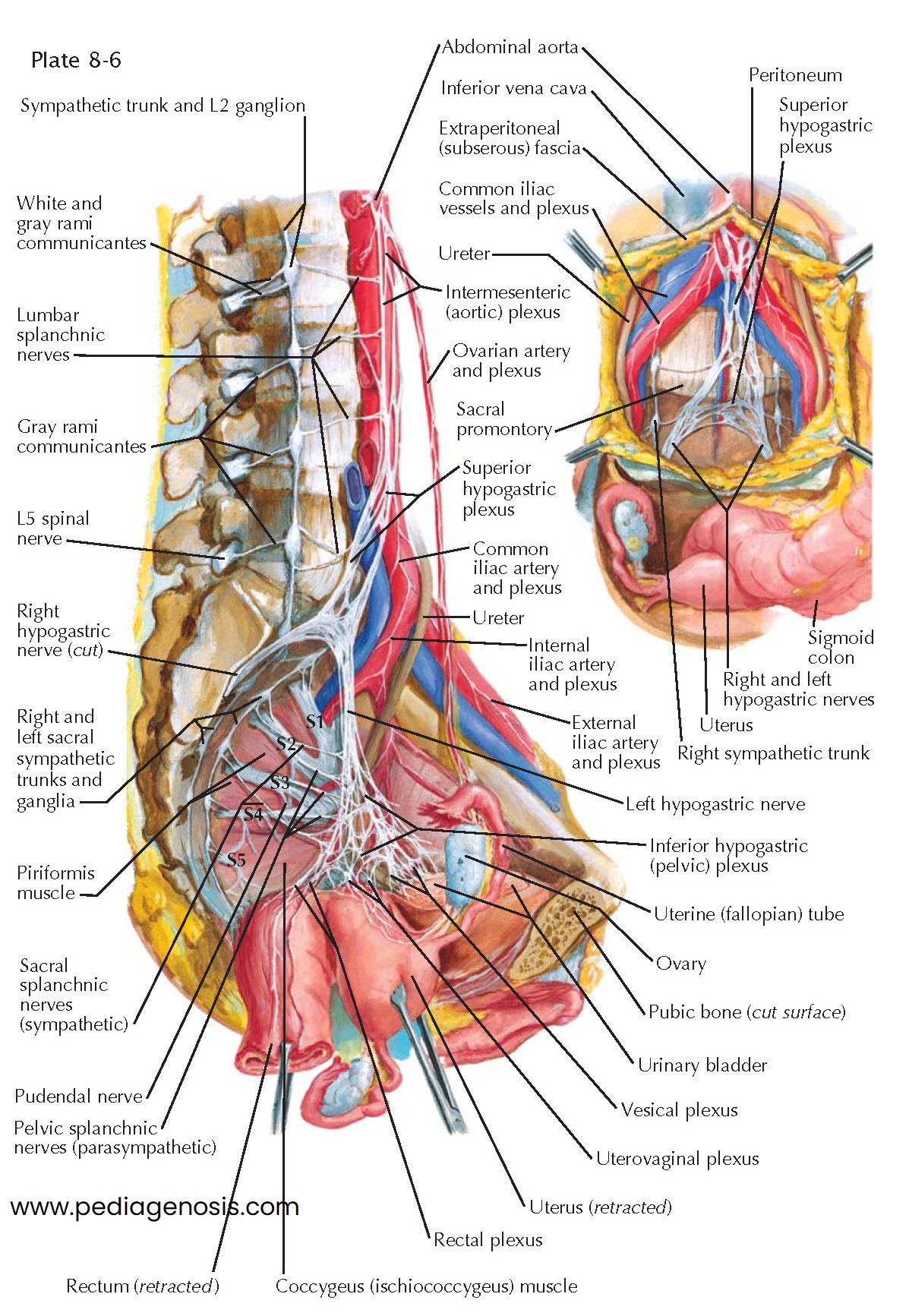
INNERVATION OF INTERNAL GENITALIA
The pelvic organs are predominantly supplied by the autonomic nervous system. The sympathetic portion of the autonomic nervous system originates in the thoracic and lumbar portions of the spinal cord, and sympathetic ganglia are located adjacent to the central nervous system. In contrast, the parasympathetic portion originates in cranial nerves and the middle three sacral segments of the cord, and the ganglia are located near the visceral organs. Although the fibers of both sub- divisions of the autonomic nervous system frequently are intermingled in the same peripheral nerves, their physiologic actions are usually directly antagonistic: sympathetic fibers in the female pelvis produce smooth muscle contraction, including the smooth muscle of the vascular system (vasoconstriction), whereas parasympathetic fibers cause the opposite effect on muscles and vasodilation.
Although autonomic nerve fibers enter the pelvis by several routes, the
majority are contained in the superior hypogastric plexus, a caudal extension
of the aortic and inferior mesenteric plexuses. From the inferior aspect of the
celiac plexus at the level of the superior mesenteric artery, two or three
intermesenteric nerves, connected by communicating branches, descend over the
anterolateral surface of the aorta, receiving fibers from the inferior
mesenteric and lumbar sympathetic ganglia. At the bifurcation of the aorta,
they join to form the superior hypogastric plexus or presacral nerve. The
superior hypogastric plexus is found in the retro- peritoneal connective
tissue. It extends from the fourth lumbar vertebra to the hollow over the
sacrum. In its lower portion, the plexus divides to form the two hypo- gastric
nerves that run laterally and inferiorly. These pass downward and laterally
near the sacral end of each uterosacral ligament and then forward over the lateral
aspect of the rectal ampulla and upper vagina. In this vicinity they are known
as the pelvic plexuses. These nerves spread out to form the inferior
hypogastric plexus in the area just below the bifurcation of the common iliac
arteries. A middle hypogastric plexus, overlying and just below the sacral
promontory, may sometimes be present.
Each pelvic plexus is composed of interlacing nerve fibers and numerous
minute ganglia, spread over an area of 2 or 3 cm2. They receive branches from
the sacral ganglia of the sympathetic trunk and parasympathetic fibers from the
second, third, and fourth sacral spinal nerves (nervi erigentes or pelvic
nerves). The pelvic plexus of nerves is subdivided into secondary plexuses,
which follow the course of the visceral branches of the hypogastric vessels.
These include the rectal plexus (to rectum), the uterovaginal plexus (to inner
aspect of fallopian tubes, uterus, vagina, and erectile tissue of vestibular
bulb), and the vesical plexus (to bladder).
The ovarian plexuses are composed of a meshwork of nerve fibers, which
arise from the aortic and renal plexuses and accompany the ovarian vessels to
supply the ovaries, the outer aspect of the fallopian tubes, and the broad
ligaments.
The anatomic relations of the presacral nerve, or superior hypogastric plexus, are of importance because its resection is sometimes performed for the relief of intractable pelvic pain. Beneath the peritoneum at the level of the bifurcation of the aorta, the superior hypogastric plexus will be found embedded in loose areolar tissue, overlying the middle sacral vessels and the bodies of the fourth and fifth lumbar vertebrae. Usually, a broad, flattened plexus, consisting of two or three incompletely fused trunks, is found. In 20% to 24% of cases, a single nerve is present. Fine nerve strands pass from the lumbar sympathetic ganglia beneath the common iliac vessels to the presacral nerve. The right ureter is visualized as it courses over the iliac vessels at the brim of the pelvis.