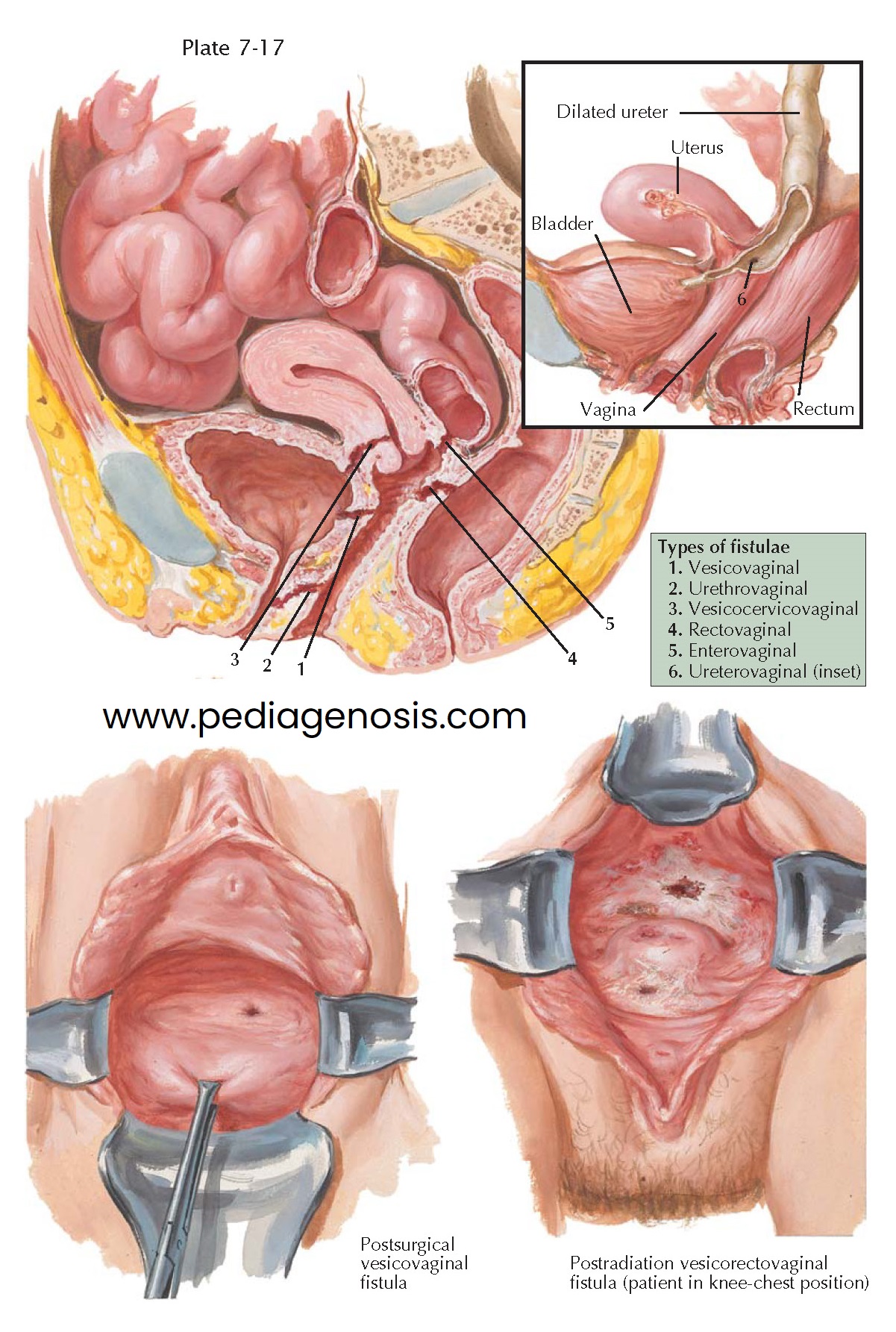
FISTULAE
A fistula is an abnormal communication between two cavities or organs. In gynecology, this usually refers to a communication between the gastrointestinal or urinary tracts and genital tract. Because of its anatomic location in close apposition to the bladder and rectum, the vagina is occasionally the site of fistulae, which divert the urinary and fecal streams, causing incontinence. These fistulae may occur in any part of the vaginal canal and are sometimes multiple.
Urinary tract fistulae may result from surgical or obstetric trauma,
irradiation, or malignancy, although the most common cause by far is unrecognized
surgical trauma. Roughly 75% of urinary tract fistulae occur after abdominal
hysterectomy. Urinary tract fistulae are most common after uncomplicated
hysterectomy, although pelvic adhesive disease, endometriosis, or pelvic tumors
increase the individual risk. Signs of a urinary fistula (watery discharge)
usually occur from 5 to 30 days after surgery (average 8 to 12), although they
may be present in the immediate postoperative period. If the defect is small,
it may spontaneously heal with simple catheter drainage (20% to 30% of
patients). More severe defects should not be repaired until the tissues have
returned to normal condition. Final repair may be by the transvaginal,
transvesical, or transperitoneal routes, depending on the size and position of
the opening. Cystoscopy may be required to evaluate the location of a urinary
tract fistula in relation to the ureteral opening and bladder trigone and to
exclude the possibility of multiple fistulae.
The majority of urethrovaginal fistulae are due to obstetric injury.
However, they may be congenital, the most common form being hypospadia. Unlike
vesicovaginal fistulae, which almost invariably cause urinary incontinence,
urethrovaginal fistulae may be associated with no symptoms, especially if the
defect is located well forward of the vesical neck.
Vesicocervicovaginal fistulae are relatively uncommon and are usually
caused by cancer of the cervix or surgical injury to the bladder in the course
of a subtotal hysterectomy. A fistulous tract in this area is often difficult to
identify and to close.
Fistulae between the gastrointestinal tract and vagina may be
precipitated by the same injuries that cause genitourinary fistulae; most common
are obstetric injuries and complications of episiotomies (lower one-third of
vagina). Fistulae may also follow hysterectomy or enterocele repair (upper
one-third of vagina). Inflammatory bowel disease or pelvic radiation therapy may
hasten or precipitate fistula formation. Although Crohn disease, lymphogranuloma
venereum, or tuberculosis are recognized risk factors, these are uncommon. For
those that do not heal spontaneously (75% of fistulae), the only effective
treatment is surgical. Repair of these fistulae may necessitate diversion of the
fecal stream by colostomy prior to definitive closure. The scarring and
puckering of surrounding tissues produced by radiation therapy greatly reduces
the chances of successful closure. Such lesions must always be biopsied to rule out the possibility of residual malignancy. Surgical treatment of these
defects is complicated, because the underlying pathologic process is usually
still progressing and the results are poor.
Surgical mismanagement accounts for most ureterovaginal fistulae. In the
course of hysterectomy, the ureter may be compressed by clamp or suture just
before it enters the bladder wall, resulting in obstruction, necrosis, and
formation of a new urinary outlet through the upper
vagina. Urinary incontinence of this type can be differentiated from that due
to vesicovaginal fistula by observing the vagina after the introduction of a dye
into the bladder. Ureterovaginal fistulae are of serious significance because
measures to restore the continuity of the urinary tract may be unsuccessful
with loss of the involved kidney.
Occasionally, a combined vesicorectovaginal fistula converts the vagina into a cloaca.