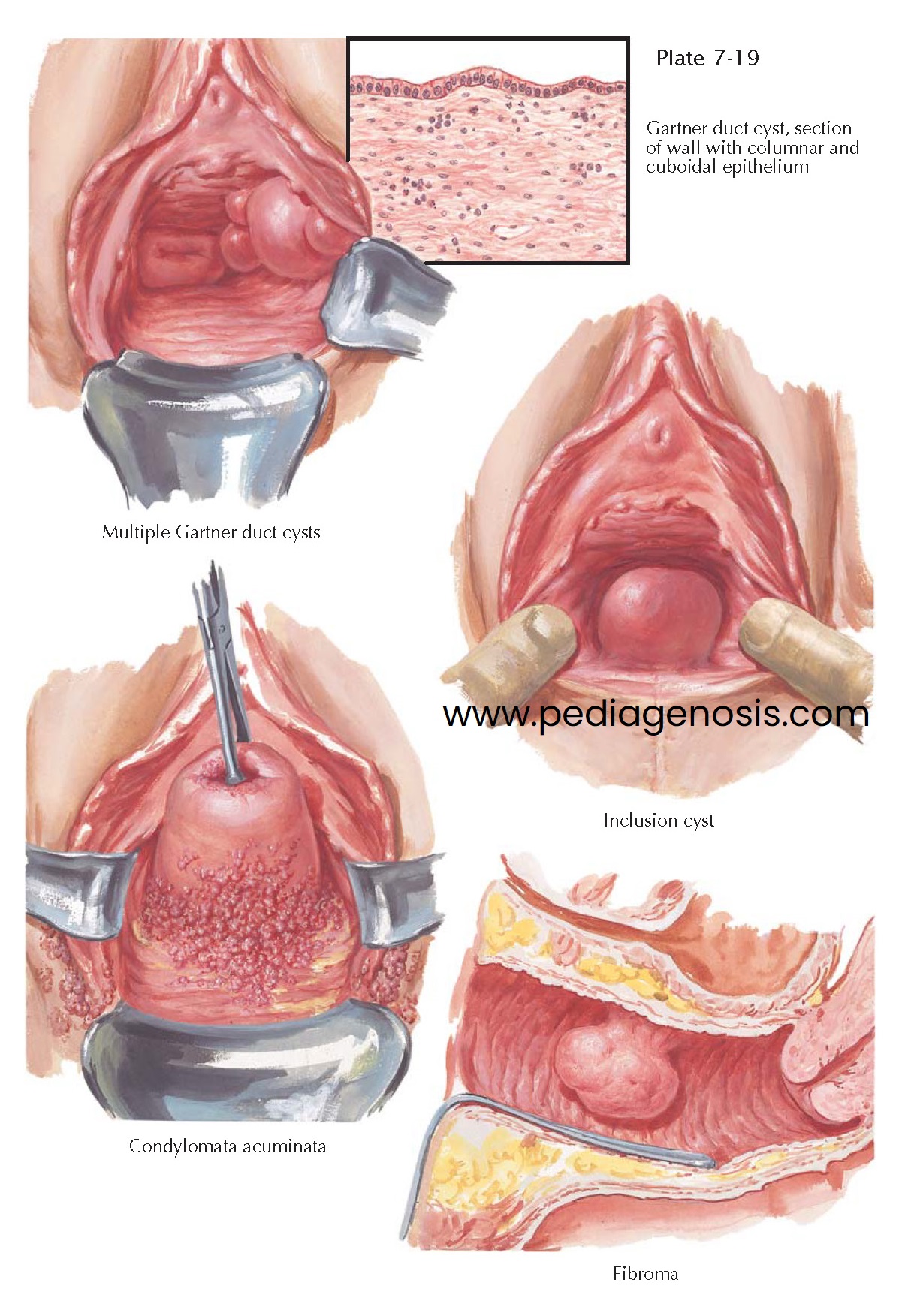
CYSTS AND BENIGN TUMORS
Vaginal tumors are relatively rare, but it is likely that the actual occurrence is more common than recognized, because many of these tumors are asymptomatic and therefore go unnoticed and untreated. Benign tumors are more prevalent than malignant and, of these, cysts are the most prevalent. Vaginal cysts are formed chiefly from embryonic epithelial remnants, which may be derived from either the müllerian or wolffian ducts, the latter giving rise to the Gartner duct cysts found on the anterolateral vaginal walls. Gartner duct cysts are blind pouches formed at the branching lower ends of the primitive mesonephric tubules. They may be single or multiple and seldom attain large size. Occasionally, a cyst of this type is large enough to occlude the vaginal canal and resemble a cystocele. In such cases, the patient may have pain, dyspareunia, bladder pressure, or even dystocia during parturition. Because the wolffian duct crosses the anlagen of the broad ligament and the uterus before entering the anterolateral vaginal wall, it is not unusual for cysts of mesonephric origin to extend well upward between the leaves of the broad ligament, increasing the hazard of surgical excision. These cysts, often an incidental finding on routine pelvic examination, need not always be excised, although some uncertainty as to the exact histologic nature of the lesion must exist when the physician decides on conservative management. The histologic architecture is extremely variable. The epithelial lining may consist of a single layer of cuboidal or high columnar epithelium, or either of these types may be stratified. Occasionally, they are lined by stratified squamous epithelium. A few inflammatory cells may be present in the stroma, and, in a very rare exception, the cyst may undergo acute infection and suppuration but never malignant degeneration.
Congenital cysts of müllerian origin may occur in the fornices or lower
in the vagina and are often referred to as inclusion cysts. They are remnants
that have been pushed aside and buried by the advancing superficial epithelium
of the urogenital sinus. Some inclusion cysts are formed when the adult vaginal
epithelium is turned into the subepithelial tissues as a result of the trauma
of delivery or vaginal surgery. These are usually in the posterior wall near
the introitus. Inclusion cysts average less than 1 cm in diameter and are
seldom larger than 3 cm. They are often asymptomatic but may cause dyspareunia
or make the patient conscious of the presence of a lump. The excised specimens
are usually of bluish color and firm consistency and, when opened, contain
thick, glairy mucus in contrast to the thin secretion of Gartner duct cysts.
The lining cells may be columnar or squamous. Inclusion cysts can be easily
removed but, when asymptomatic, need no
treatment.
Papilloma and condylomata acuminata occur in the vagina as well as on the
external genitalia. Their gross and microscopic characteristics are not modified
by their vaginal location. Condylomata are grouped near the vestibule on the
posterior and lateral walls or high in the posterior fornix. They produce a
foul discharge, especially when they become large and infected, and must be
carefully differentiated from malignancy and the venereal granulomas before
appropriate treatment is instituted. Local application of podophyllin, trichloroacetic acid, or other topical therapies eradicates the majority
of small lesions.
Fibroma and myoma are quite common in the vagina but are seldom of a size
sufficient to produce symptoms. The rare case may be large and pedunculated.
These tumors are usually insensitive but may occasionally cause local
discomfort. Surgical excision is indicated, since malignancy cannot be excluded
grossly.
Other benign vaginal tumors, such as lymphangioma and mole, are extremely rare.