ASHERMAN SYNDROME (UTERINE SYNECHIA)
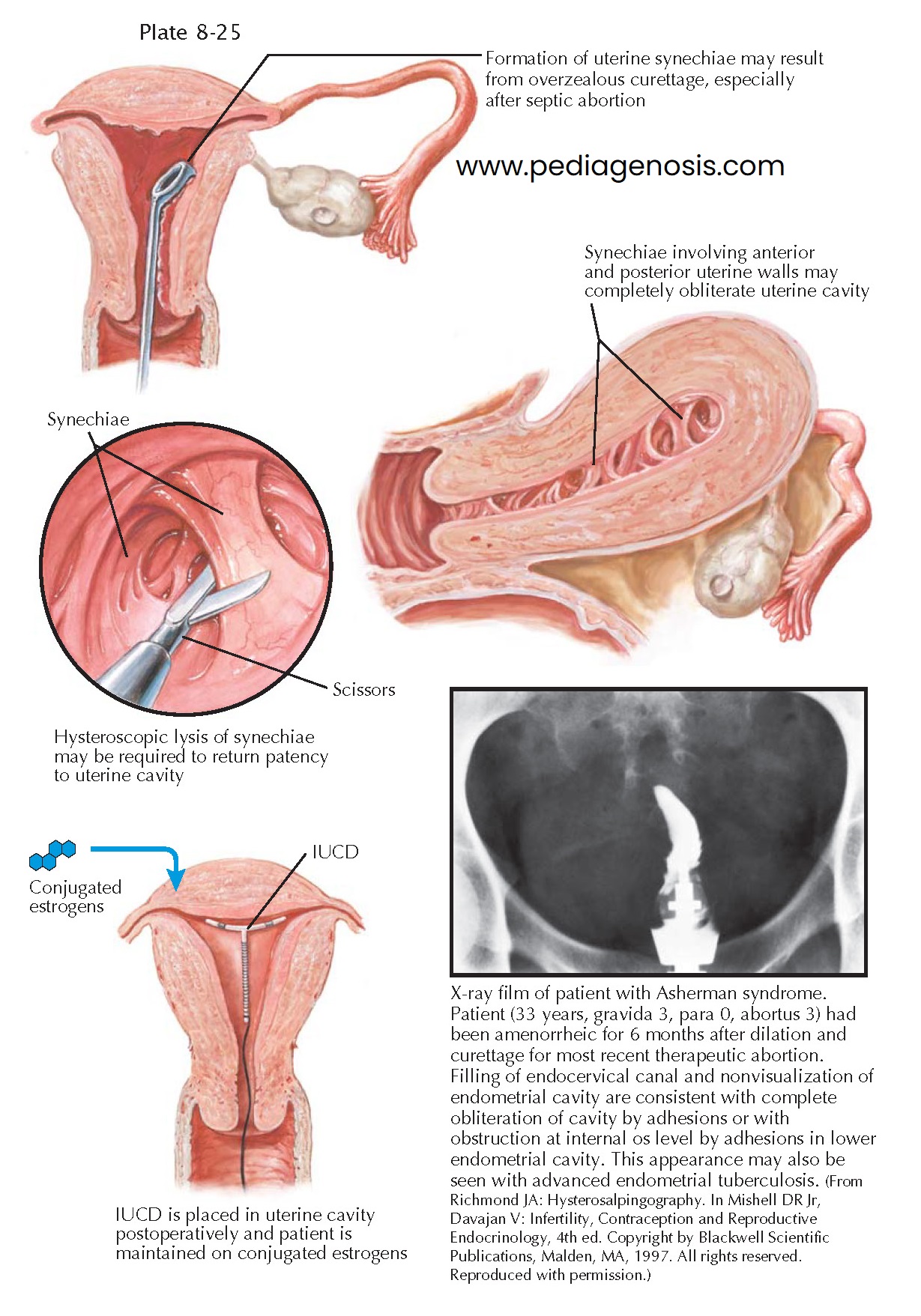 |
Asherman syndrome (uterine synechia) is scarring or occlusion of the uterine cavity after curettage, especially when surgery is performed after septic abortion or in the immediate postpartum period. (Though the same changes occur following therapeutic endometrial ablation, the term is generally not applied in that setting.) This scarring generally results from endometrial damage involving the basal layers (normal curettage, excessive curettage, curettage when infection is present or in the immediate postpartum period—some intra-uterine adhesions form in 30% of patients treated by curettage for missed abortion), or endometrial infection (tuberculosis or schistosomiasis). More than 90% of the cases occur following pregnancy-related curettage. A severe pelvic infection unrelated to surgery, including endometrial tuberculosis infections, may also lead to Asherman syndrome. (Chronic endometritis from genital tuberculosis is a significant cause of severe intra-uterine scarring in the developing world, often resulting in total obliteration of the uterine cavity.) A less common cause of IUA is severe endometritis or fibrosis following a myomectomy, metroplasty, or cesarean delivery. In some cases, the whole cavity may be scarred and occluded, resulting in secondary amenorrhea. Even with relatively few scars, the endometrium may fail to respond to estrogens, which means that there is a poor correlation between symptoms and the severity of scarring found.
The true prevalence of Asherman syndrome is unclear because of a lack of
awareness of the symptoms or diagnosis and the nonspecific nature of the
symptoms. Intrauterine scarring is estimated to affect 1.5% of women undergoing
hysterosalpingography, between 5% and 39% of women with recurrent miscarriage,
and up to 40% of patients who have undergone curettage for retained products of
conception (incomplete abortion).
Patients with uterine synechia generally present with amenorrhea,
hypomenorrhea, recurrent early pregnancy loss, or infertility depending on the
extent and intrauterine location of adhesions. Pain during menstruation and
ovulation is also sometimes experienced, and can be attributed to sequestration
and obstruction. Most often the patient will have a history of one or more risk
factors such as curettage or infection, and the temporal relation between these
events and the onset of symptoms should be suggestive of intrauterine scar-
ring. Hysteroscopy, sonohysterography, or hysterosalpingography may all be used
to confirm the diagnosis. Ultrasonography, without the use of saline infusion,
is not a reliable method of diagnosing intrauterine scarring. It has been suggested
that sequential administration of estrogen followed by progestogen can be used
as the initial diagnostic procedure when intra-uterine scarring is suspected. Unfortunately, withdrawal bleeding occurs
following administration of the steroids in most women with intrauterine
adhesions, resulting in a lack of specificity of this approach. If left untreated, retrograde menstruation (if present) caused by outflow
obstruction may result in the development of endometriosis.
When uterine synechiae are diagnosed, resection of intrauterine scars
under hysteroscopic control (sometimes with laparoscopy used as a protective
measure against uterine perforation), followed by intrauterine contraceptive
device (IUCD) insertion and estrogen therapy may be
curative, providing a return of normal menstrual function and fertility.
Repeated scarring may occur in up to 50% of cases, necessitating postoperative
follow-up or repeated treatment. For this reason, follow-up tests, including a
hysterosalpingogram, hysteroscopy, or sonohysterography, are necessary to
ensure that scars have not reformed. Patients who have undergone resection of
intrauterine adhesions who subsequently become pregnant are at greater risk for having abnormal placentation, including placenta accreta.
The prognosis for these patients is a function of the initial severity: Small scars can usually be treated with success; extensive obliteration of the uterine cavity or fallopian tube ostia may require several surgical inter-ventions or even be uncorrectable. In these cases, surrogacy, in vitro fertili ation (IVF), or adoption may be the only alternatives.




