VITAMIN K DEFICIENCY AND VITAMIN K ANTAGONISTS
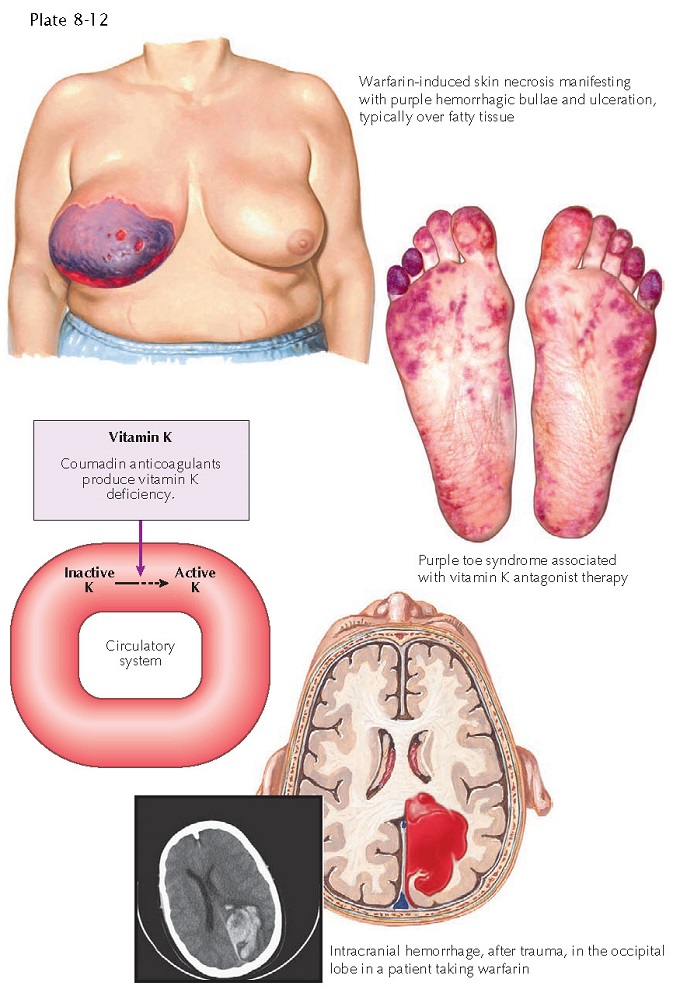 |
| POTENTIAL CLINICAL CONSEQUENCES OF WARFARIN USE |
Vitamin K is an essential nutrient that is required as a cofactor for the production of a handful of coagulation cascade proteins. It is a fat-soluble vitamin that is efficiently stored in the human body. Vitamin K deficiency is rare and is typically seen only transiently in neonates and infants during the first 6 months of life. Affected neonates may show abnormally prolonged bleeding after minor trauma. Patients may have an elevated pro- thrombin time (PT) and decreased serum levels of vitamin K and coagulation factors. Therapy consists of replacement of vitamin K to normal levels and a search for any possible underlying cause, such as liver or gastrointestinal disease. Neonatal and infantile vitamin K deficiency is most likely caused by maternal breast milk insufficiency of vitamin K.
Vitamin K
deficiency is rarely seen in adults, because most diets contain enough vitamin
K for normal physiological functioning. Adult patients with liver disease and
malabsorption states are at highest risk for the development of vitamin K
deficiency. Vitamin K may be found in two natural forms: vitamin K1
(phylloquinone) and vitamin K2 (menaquinone). K1 is found in plants, and K2 is
produced by various bacteria that make up the normal flora of the
gastrointestinal tract. Anti- biotics may cause a decrease in the bacterial
production of vitamin K2, resulting in a lack of vitamin K available for
absorption. This is typically not a clinical issue unless the patient is taking
a vitamin K antagonist such as warfarin. Vitamin K is absorbed in the distal
jejunum and ileum via passive diffusion across the cell membrane. The
majority of vitamin K is stored normally in the liver. There, the vitamin is
converted to its active state, hydroxyquinone. An efficient vitamin K salvage
pathway normally prevents an individual from becoming deficient in the vitamin.
The enzyme vitamin K epoxide reductase is responsible for converting the
inactive epoxiquinone to the active hydroxyquinone form of vitamin K.
Warfarin is
a synthetic analogue of vitamin K and is the main vitamin K antagonist. It is indicated for use as an
anticoagulant in the treatment of a number of conditions, including atrial
fibrillation and deep venous thrombosis, and after heart valve replacement
surgery. Warfarin acts by inhibiting the enzymes that are responsible for
carboxylation of glutamate residues and epoxide reductase. This both decreases
the available clotting factors and induces vitamin K deficiency, leading to
added reduction of available clotting factors. Clinical Findings: Vitamin
K antagonists have been shown to cause a specific type of cutaneous eruption
known as warfarin necrosis, which occurs in approximately 0.05% of patients
taking the medication. Warfarin necrosis affects the areas of the body that
have increased body fat, such as the breasts, the abdominal pannus, and the
thighs. The feet are also particularly prone to development of warfarin
necrosis. The skin initially
develops small, red to violaceous petechiae and macules preceded by
paresthesias. These regions become erythematous and purple (ecchymoses) with
intense edematous skin. The lesions eventually ulcerate or form hemorrhagic
bullae. The hemorrhagic bullae desquamate, leaving deep ulcers. Painful
cutaneous ulcers may occur, with some extending into the subcutaneous tissue,
including muscle. Most ulcers appear within 5 to 7 days after the initiation of warfarin therapy. Secondary
infection may be a cause of significant morbidity. The affected areas continue
to undergo necrosis unless the warfarin is withheld and the patient is treated
with a different class of anticoagulant. The feet and lower extremities may
have a reticulated, purplish dis- coloration called “purple toe syndrome.” This
cutaneous drug reaction can be eliminated or at least drastically decreased if the patient
is pretreated with heparin or another equivalent anticoagulant before warfarin
is initiated.
Histology:
Skin
biopsies from areas of warfarin necrosis show an ulcer with a mixed
inflammatory infiltrate. Thrombosis is seen within the small vessels (venules
and capillaries) of the cutaneous vasculature. Arterial involvement is absent.
Minimal to no inflammatory infiltrate is present. Red blood cell extravasation
is prominent. The main histopathological finding is microthrombi. Findings of
inflammation, a neutrophilic infiltrate, arterial involvement, a strong
lymphocytic infiltrate, or the presence of bacteria in or around vessels
mitigate against the diagnosis of warfarin necrosis. Bacteria will be present
on the surface of the ulcer and are believed to be a secondary phenomenon.
Pathogenesis:
Vitamin
K is needed for the modification of many coagulation cascade proteins,
including protein C, protein S, factor II (prothrombin), factor VII, factor IX,
and factor X. Factors II, VII, IX, and X are critical in forming a clot and are
produced in the liver as inactive precursors. Preactivation of these clotting
factors requires the action of vitamin K carboxylation on glutamate amino acid
residues. Once preactivated, the clotting factors are available for full
activation and clot formation when exposed to calcium and phospholipids on the
surface of platelets.
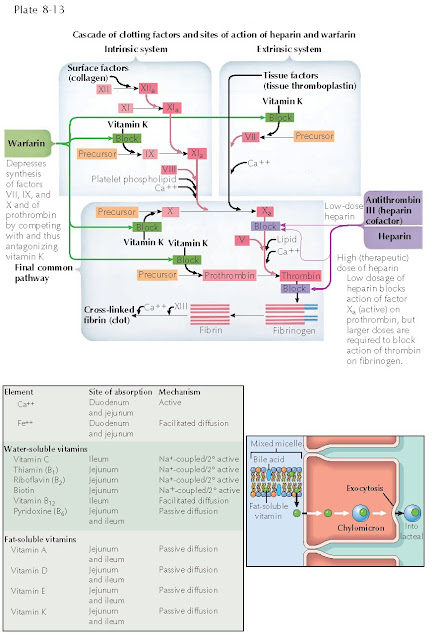 |
| ANTICOAGULATION EFFECTS ON THE CLOTTING CASCADE |
Inhibition
of these clotting factors by vitamin K antagonists leads to anticoagulation.
Warfarin works by inhibiting the carboxylation of glutamate. On the other hand,
protein C and protein S are responsible for turning off the clotting cascade
and play a natural regulatory role in normal coagulation. When these proteins
are inhibited, the clotting cascade may proceed unimpeded, allowing for
excessive clotting. Protein C and protein S have shorter half-lives than
factors II, VII, IX, and X. Therefore, when individuals are treated initially
with warfarin, the levels of protein C and protein S are depleted before the
other factors, leading to a prothrombic state.
This initial prothrombic state is responsible for the clinical signs and
symptoms of microvasculature blood clotting and skin necrosis. The clotting
takes place in areas of increased adipose tissue because of the sluggish flow
of blood through the fine vasculature in these regions. For this reason, most
patients are given heparin or a similar anticoagulant until the full effect of
warfarin on all clotting factors has occurred.
Therapy:
Treatment
of warfarin necrosis requires discontinuation of warfarin and initiation of
heparin anticoagulation and supportive care with fresh-frozen plasma and
vitamin K replace the lost protein C and protein S. Surgical debridement may be
required, and one should be vigilant for any signs or symptoms of secondary
infection. Therapy consists of proper replacement of vitamin K and supportive care. Menadione is a synthetic
form vitamin K that can be given therapeutically.
Vitamin K deficiency in neonates and infants is diagnosed by an isolated elevation in the prothrombin time. The levels of the vitamin K–dependent clotting cofactors can each be measured, and vitamin K replacement should be administered to those who are deficient. Breast milk is not a strong source of vitamin K, and if the mother had previous children with vitamin K deficiency, the newborn should be given supplemental vitamin K. The best method for supplementation has yet to be determined, but it can be achieved with a one-time intramuscular injection or with oral replacement.




