Overview of Gastrointestinal Hemorrhage
 |
| CAUSES OF GASTROINTESTINAL HEMORRHAGE |
Many gastrointestinal disorders manifest themselves by bleeding. Intestinal bleeding may present as bright-red blood, suggesting gross lower bleeding (hematochezia), passage of black stool (melena), or other findings of bleeding but no change in stool color (occult bleeding). When no cause of bleeding can be detected with the usual examinations, obscure gastrointestinal bleeding is occurring.
More
severe hemorrhages reveal themselves by the appearance of visible blood in the
stool, where it may be intermingled with the fecal material as bright-red blood
(hematochezia) or appear as bloody diarrhea. Hematochezia in small
volumes is almost always caused by a colonic lesion. In contrast, passage of
large volumes of red blood or bloody stools may be caused by intestinal
disorders or upper gastrointestinal hemorrhage, in which case it signifies
massive bleeding. It is often noted that the “most common etiology of
hemodynamically significant lower GI bleeding is an upper GI source” originating
above the ligament of Treitz. Lesions causing upper gastrointestinal bleeding
can accurately be detected in more than 95% of cases by upper endos- copy.
Upper endoscopy is a procedure of shorter duration than colonoscopy, does not
require bowel preparation, and often detects lesions that can be easily treated
by a wide variety of effective devices. If upper endoscopy is negative,
attention should be directed to the colon as the most likely source and to the
small intestine only if thorough evaluations of both the upper digestive tract
and colon are negative.
Distinguishing
upper bleeding from lower bleeding is often challenging, even for experts.
Bleeding that is at first thought to originate in the colon will later be
determined to be from an upper source in 15% of patients. An upper digestive
organ source is confirmed in patients with hematemesis,
blood in a nasogastric lavage, or blood seen endoscopically. An upper source
should be pursued before proceeding with colonoscopy whenever bleeding is brisk
and hemodynamically significant, there is melena, there is known or suspected
liver disease, the patient has been taking nonsteroidal anti-inflammatory
drugs, or there are known upper pathologic findings. Lower gastrointestinal
bleeding is less likely if the blood urea nitrogen–to-creatinine ratio is
higher than 25 and very unlikely if the ratio is higher than 50.
Substantial
bleeding may also present as black stool, known as melena. The black
color indicates that blood has been exposed to the digestive activity of
intestinal secretions, and therefore, as a rule, it is a sign that the bleeding
originates from a lesion in the gut above the cecum. Rarely, however, melena
may occur with lesions located as low as the left colon. Because colonoscopy will
detect a source of bleeding in the colon in less than 5% of patients with
melena who have had a negative endoscopic examination, it is imperative that a
thorough upper examination be performed first in all patients with melena as
well as in those with overt bleeding.
The
loss of blood from the intestines may be so minimal that, in the absence of
other symptoms, it may escape attention until microcytic anemia is seen as the
first sign of a gastrointestinal disorder. Because bleeding is often the only
sign of serious pathologic situations in the digestive tract, it is important
to include an evaluation for fecal “occult” blood at the slightest suspicion of
a lesion in the gut.
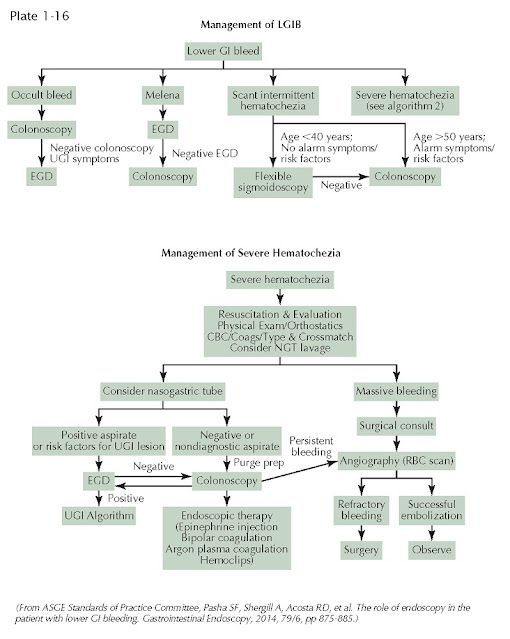 |
| MANAGEMENT OF GASTROINTESTINAL HEMORRHAGE |
To
avoid pitfalls, one should remember that neither stool color nor the presence
of blood on fecal occult blood testing is conclusive evidence that a lesion is
present in the digestive system. The stool may be discolored for reasons other
than the presence of blood. The stool is often gray or black in patients taking
iron or bismuth preparations. It may be reddish when the patient has eaten
beets or other red substances if transit is rapid, as occurs with severe
diarrhea. Likewise it is important to appreciate that bleeding originating in
the oral or pharyngeal cavity or from hemorrhagic lesions in
the respiratory tract can be detected in the feces. Vaginal bleeding may
also be mistaken as rectal bleeding. More commonly, false-positive testing for
occult blood occurs in patients eating red meat. Such false-positive results
can be avoided if testing is performed with immune techniques that accurately
detect only human hemoglobin.
Before
proceeding with definitive testing and possible treatment with endoscopic
techniques, the airway, breathing, and circulatory status of the patient must
be promptly assessed and secured (ABCs of emergency care). The history should
focus on potential causes, the volume of blood lost, the presence of any signs
or symptoms of coagulopathy (including use of nonsteroidal
antiinflammatory drugs), and the presence of comorbidities. Correcting any of
these existing problems must be the foremost priority during the first 24 hours
after the patient is admitted to the hospital. Laboratory testing, including a
complete metabolic panel, complete blood count, and coagulation studies, should
be sent for stat analysis. Blood should be drawn for blood typing and, when
appropriate, for cross-matching. Only when the patient is hemodynamically
stable and any ongoing concurrent illnesses have been addressed and optimized
should the bowel be thoroughly prepped for an urgent colonoscopic examination.
The
source of lower gastrointestinal bleeding can be accurately detected in most
patients by colonoscopy. In a select
clinical setting, particularly when the patient has recently had a normal
colonoscopy and describes low-volume hematochezia, a sigmoidoscopy may be all
that is needed. It is particularly useful to perform sigmoidoscopy when the
patient is actively experiencing bleeding. Hemorrhoids missed by flexible
endoscopic techniques may be more accurately detected with rigid proctoscopy.
When upper endoscopy and colonoscopy fail to identify a source,
balloon-assisted enteroscopy can reach most, if not all, of the jejunum and
ileum. Sources of bleeding can often be treated using these endoscopic
techniques. The use of other techniques to detect bleeding sources, including
capsule enteroscopy, nuclear scans, angiography, and cross-sectional imaging techniques,
is described in Plates 2-12 and 2-33.




