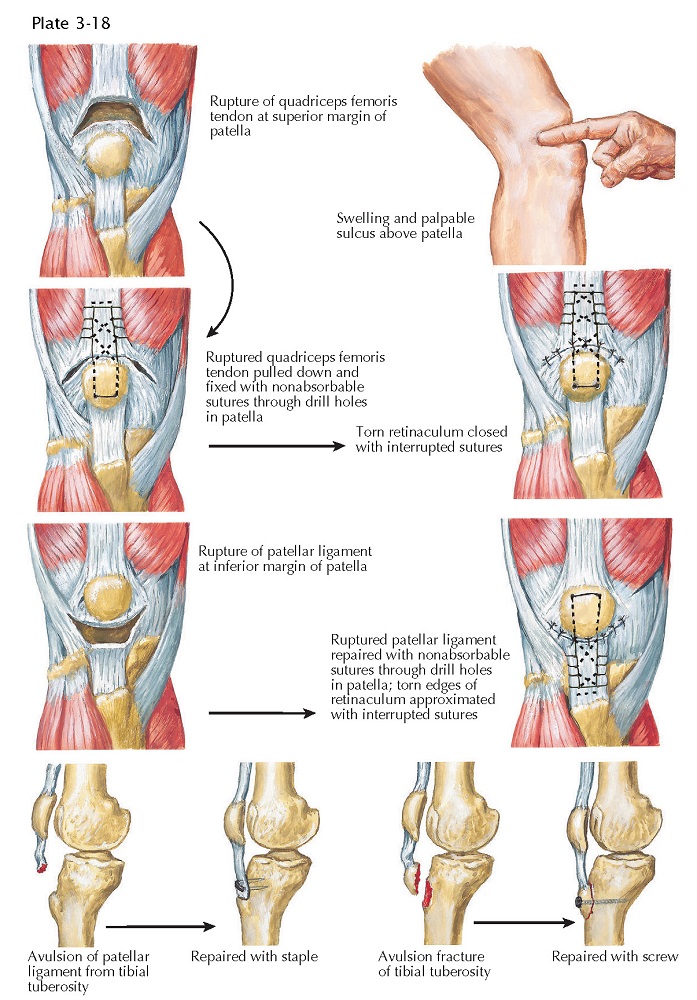
DISRUPTION OF QUADRICEPS FEMORIS
TENDON OR PATELLAR
LIGAMENT
Damage to the quadriceps mechanism generally occurs when there is active contraction of the quadriceps femoris muscle against forced flexion of the knee. Most ruptures of this extensor mechanism occur in older patients. At the time of injury, the patient experiences sudden pain, which may be associated with a tearing sensation about the knee. The tendon may be weakened by age-related degenerative changes or by pathologic changes due to psoriatic arthritis, rheumatoid arthritis, arteriosclerosis, gout, hyperparathyroidism, diabetes, chronic renal failure, or corticosteroid therapy.
Physical Examination. Palpation of the knee
often reveals a hematoma, which may make examination difficult. A high-riding
patella may indicate rupture of the patellar ligament, whereas a patella that
is riding lower than normal suggests a rupture of the quadriceps femoris
tendon. A large defect may be palpable soon after injury, although if the
ruptured ligament is not treated for weeks or months the sulcus may fill with
scar tissue.
The most important finding during examination is the patient’s inability
to actively extend the knee fully against gravity. Also, the patient may not be
able to maintain a passively extended knee against gravity. Patients with
rupture of the quadriceps femoris tendon or patellar ligament without
involvement of the medial or lateral retinaculum may be able to extend the
injured knee actively to within 10 degrees of full extension. When there is a
widely separated tear of either tendon or ligament combined with involvement of
the medial and lateral retinacula, active extension is very difficult. Patients
with chronic rupture of the quadriceps femoris tendon complain of giving way of
the knee and marked weakness on attempting active extension.
Imaging. Whereas physical examination is often sufficient to
diagnose disruptions of the extensor mechanism, it is recommended to obtain
plain radiographs to assess for fracture and patellar positioning. MRI may be
performed to assess the involved soft tissues in detail, although this is not
often necessary for these patients. Treatment. Rupture of the
quadriceps femoris tendon generally occurs at its point of intersection into
the superior pole of the patella, whereas rupture of the patellar ligament
usually occurs at the inferior pole of the patella. In both cases, surgery is
required to reestablish the continuity of the quadriceps mechanism. The tendon
or ligament most often is reattached with sutures through drill holes in the
patella. Then, the medial and lateral retinacula are sutured. After surgery,
the knee is routinely immobilized in full extension for 6 to 8 weeks.
Patients who also have chronic metabolic disorders or receive long-term
corticosteroid treatment may require a more complex repair that uses tendon,
fascia, or wire to reinforce the damaged quadriceps mechanism. After
postoperative immobilization for 8 to 10 weeks, patients gradually start
protected range-of-motion exercises and should use a cane or walker for some
time.
Rupture of the patellar ligament may also occur at its insertion on the tibia, with or without fracture of the tibial tuberosity. In children whose growth plates have not yet closed, the ligament should be sutured, because this injury may disturb the growth of the proximal tibia. In adults, avulsion of the ligament from the tibial tuberosity is repaired by suturing the avulsed ligament though drill holes in the tibia or securing it with a metal staple or screw. A displaced fracture of the tibial tuberosity may be treated with open reduction and fixation with a metal screw.