DISLOCATION OF KNEE JOINT
Dislocation of the knee joint must be distinguished from dislocation of the patella. Whereas a patella dislocation involves the patellofemoral joint, a knee dislocation involves the tibiofemoral articulation. Any dislocation is an emergency, and dislocation of the knee is no exception. Reduction should be achieved as soon as possible. Striking the knee against the dashboard during an automobile accident is the most common cause of injury, but athletic injuries are also common causes. The popliteal artery and its branches are often damaged during dislocation of the knee. Therefore, arterial injury must be suspected in every knee dislocation. A thorough neurovascular examination should be performed before and after reduction, and an ankle- brachial index (ABI) should be obtained as well. If there remains any question of arterial damage, the patient frequently will undergo arteriography or CT angiography and any necessary arterial repair should be done immediately.
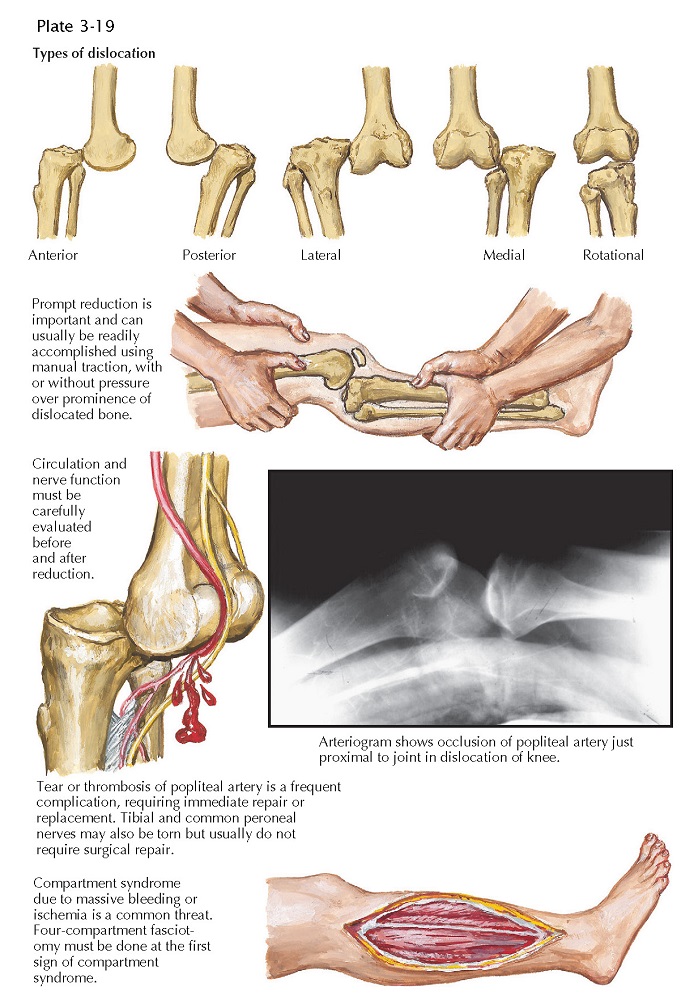
Classification of knee dislocations is based on the position of the
tibia in relation to the femur. In an anterior dislocation of the knee the
tibia is anterior to the femur, whereas in a posterior dislocation the tibia is
posterior to the femur. Lateral, medial, and rotational dislocations may also
occur, as may combination patterns such as anterolateral and posterolateral.
Associated vascular injuries are more common with anterior dislocations,
whereas the peroneal nerve is more likely to be injured in posterolateral
dislocations.
Diagnosis of dislocation of the knee is based on the patient’s history
and typical clinical findings. If the dis- location has not spontaneously
reduced before the patient is examined, the diagnosis is clear because the
deformity is obvious and impressive. However, spontaneous reduction of knee
dislocations is common. When gross dislocation is not detected by physical
examination or radiography but there is a history of significant knee injury, a
dislocation that has spontaneously reduced may be suspected. A large effusion
or hemarthrosis may not develop because large tears in the joint capsule allow
the fluid to escape into the soft tissues about the knee.
The initial treatment of a knee dislocation is straight-forward but must
begin without delay. Reduction is performed using gentle longitudinal traction
and is frequently accomplished with little or no sedation. If any difficulty at
all is encountered, anesthesia should be induced promptly. After reduction, the
neurovascular status of the limb must be carefully monitored.
Many knee dislocations are treated with splinting or casting, but
because the reduced knee is so unstable, it is difficult
to keep the joint surfaces in proper apposition without surgical stabilization.
Once the patient is hemodynamically stable, it is common to obtain an MRI to
assess for ligamentous and soft tissue injury. Early surgical repair of torn
ligaments and joint capsule may then be performed. In cases of severe
instability, the knee can temporarily be stabilized with an external fixator or
internally with pins or plates. Surgical repair maintains the reduction and may
provide long-term stability after this devastating injury.
The trifurcation of the popliteal artery is tethered to the leg where
the anterior tibial artery goes through a gap in the interosseous membrane. In
anterior dislocations, stretching of the artery and vein is severe and often
results in vascular injury. If dislocation is not reduced and if the vascular
supply is cut off for hours, reduction and restoration of vascular flow may be
accompanied by the development of a compartment syndrome, which is a serious
complication with often irreversible consequences.