URETEROSCOPY
Ureteroscopy refers to the direct visualization of the ureter and renal pelvis using an endoscope. It is indicated for the treatment of numerous conditions, including renal and ureteral stones, ureteropelvic junction obstructions, ureteral strictures, and upper tract malignancies. It may also be performed to remove foreign bodies, such as a proximally migrated ureteral stent. Finally, it may be performed to evaluate abnormal urine cytology findings, filling defects on retrograde pyelography, or hematuria.
URETEROSCOPE
DESIGN
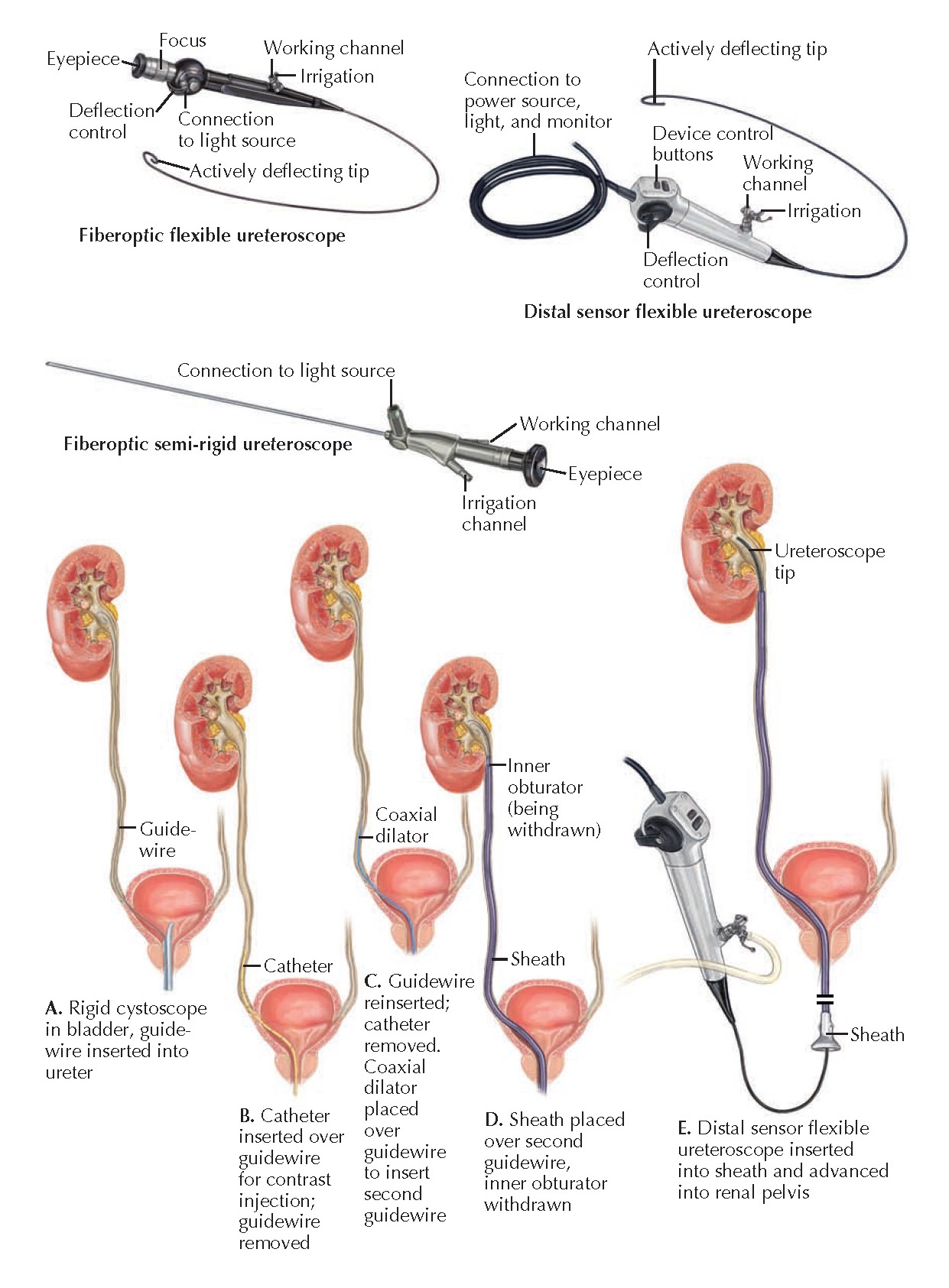
Ureteroscopes
are small endoscopes that can be either semirigid (minimal bending of the
straight metal shaft) or flexible (with an actively or passively deflectable
distal tip). Both types feature optics consisting of either fiberoptic bundles
or, more recently, a distal sensor. All ureteroscopes have at least one working
channel, which is used for irrigation and through which laser fibers, stone
baskets, and other devices may also be deployed. The size (outer diameter) of a
ureteroscope is given in the French scale (1 Fr 0.33 mm).
 |
| Plate 10-33 URETEROSCOPY: DEVICE DESIGN AND DEPLOYMENT |
Semirigid ureteroscopes are primarily used to diagnose or treat pathology in the mid to distal ureter (i.e., below the iliac vessels). They have a tapered distal tip and typically possess one large working channel or two smaller working channels. The advantages of semirigid ureteroscopes over flexible ureteroscopes include larger working channels, improved stability in the distal ureter, and easier ureteral access. Disadvantages include the potential for urethral trauma during ureteroscope insertion, as well the potential for ureteral trauma during intubation of the ureteric orifice and manipulation of the ureteroscope within the ureter.
Flexible
ureteroscopes can be used to access any area of the upper urinary tract, but
they are primarily used to access the proximal ureter (i.e., above the iliac
vessels) and renal pelvis. Contemporary flexible ureteroscopes provide dual
deflecting capability of approximately 120 to 170 degrees in one direction and
170 to 270 degrees in the other direction, controlled using a thumb- operated
lever. At present, all flexible ureteroscopes have a single working channel. The
flexibility of the ureteroscope decreases when an instrument is present in the
working channel; however, small-diameter holmium laser fibers have been
developed that are both flexible and durable, causing only minimal resistance
during deflection.
TECHNIQUE
Before
undergoing ureteroscopy, the patient should have a documented negative
urinalysis and urine culture, so as to reduce the risk of urosepsis.
The majority
of ureteroscopic procedures are performed in a specialized cystoscopy suite.
The patient is placed
in a dorsal lithotomy position, with the lower extremities in stirrups. Either general or regional
anesthesia is employed.
The
procedure is typically initiated by visualizing the bladder lumen with a
cystoscope (see Plate 10-37) and then deploying a guide wire into the ureteric
orifice. The guidewire may be placed with either a rigid or flexible cystoscope,
depending on surgeon preference. Next, a ureteral catheter is inserted over the
wire, and a retrograde pyeloureterogram is performed to evaluate the anatomy of the upper
tract and provide a map for deployment of the ureteroscope.
After the
ureteral catheter has been withdrawn, the ureteroscope can be deployed. A
semirigid uretero- scope is inserted adjacent to the wire. The wire, which
provides a map of the upper urinary tract, can remain in place throughout the
procedure. A flexible ureteroscope, in contrast, is deployed over the wire. Once
it is in position, the wire must be withdrawn from the working channel to permit normal deflection and the introduction of
devices. Thus before deployment of a flexible ureteroscope, a second guide wire
is typically inserted to act as a “safety” wire, which remains present
throughout the entire procedure and provides access to the upper urinary tract
should normal anatomy become disrupted. To place a safety wire, a coaxial
dilator/ sheath is introduced over the first wire. The inner dilator is removed,
the safety wire is introduced through the sheath, and then the sheath is
removed.
When a
flexible ureteroscope is being used, a ureteral access sheath can be placed
early on to facilitate multiple insertions of the ureteroscope and limit the
trauma associated with each passage. These sheaths also facilitate drainage of
irrigation fluid, therefore permitting more frequent flushing of stone fragments
and other debris created during lithotripsy procedures. Many different sheaths
are available with a wide range of diameters and lengths. A ureteral access
sheath is introduced over a wire. A tapered inner obturator in its lumen
facilitates its passage through the ureter and helps dilate narrowed regions
that would otherwise be difficult to traverse. Once the sheath is in position,
the inner obturator and guide wire are removed. The ureteroscope can then be
deployed through the sheath lumen. At the end of the procedure, the sheath is
removed under direct vision.
As the
ureteroscope is advanced to the desired position, fluoroscopy is performed to
monitor its progress in real time. Throughout the process, the urinary tract is
irrigated with saline to facilitate ureteroscope passage and improve
visualization. Irrigation pressure can be controlled by gravity, a compression
bag, or hand-held pumps. If passage of the ureteroscope is difficult, the ureter
may be dilated by passing a balloon dilator over the guide wire. Once the
ureteroscope has reached the level of interest, various instruments can be
introduced into the working channel to perform a diagnostic (e.g., biopsy) or
therapeutic (e.g., ablation, stone basketing) procedure.
At the end
of the procedure, a ureteral stent should be deployed if a ureteral access
sheath has been used because the latter is associated with a risk of mucosal
injury and postoperative ureteral edema. Ureteral stents are typically
biocompatible polyethylene or silicone polymer devices. Most stents have curls
at their proximal and distal ends, which help anchor them in the renal pelvis
and bladder. In addition, most stents have small holes along their shaft to
facilitate drainage. A ureteral stent may be placed through the working channel
of a rigid cystoscope, or it can be deployed over a wire using fluoroscopic
guidance. A plastic tube known as a stent pusher is used to ensure that the
proximal curl reaches the renal pelvis. Care must be taken not to advance the
distal curl into the ureter.
 |
| Plate 10-34 STONE FRAGMENTATION AND EXTRACTION |
COMPLICATIONS
When
performed properly, ureteroscopy is associated with few complications. The most
common complications include stent colic (discomfort from the ureteral stent),
transient hematuria, and urinary tract infection. The most concerning
complication is ureteral perforation. Most cases of ureteral perforation,
however, successfully heal with stent deployment alone. Ureteral avulsion is a
rare complication of ureteroscopy that is most often repaired using open
surgical technique.
FOLLOW-UP
Ureteroscopy
is typically performed on an outpatient basis and does not require hospital
admission. At present, there is no standard protocol for postoperative
follow-up. A typical evaluation to rule out residual stone disease or stricture
formation may include CT scan; radiograph of the kidneys, ureter, and bladder;
or renal ultrasound. If a ureteral stent is placed after an uncomplicate
ureteroscopy, it is usually removed 3 to 14 days later.




