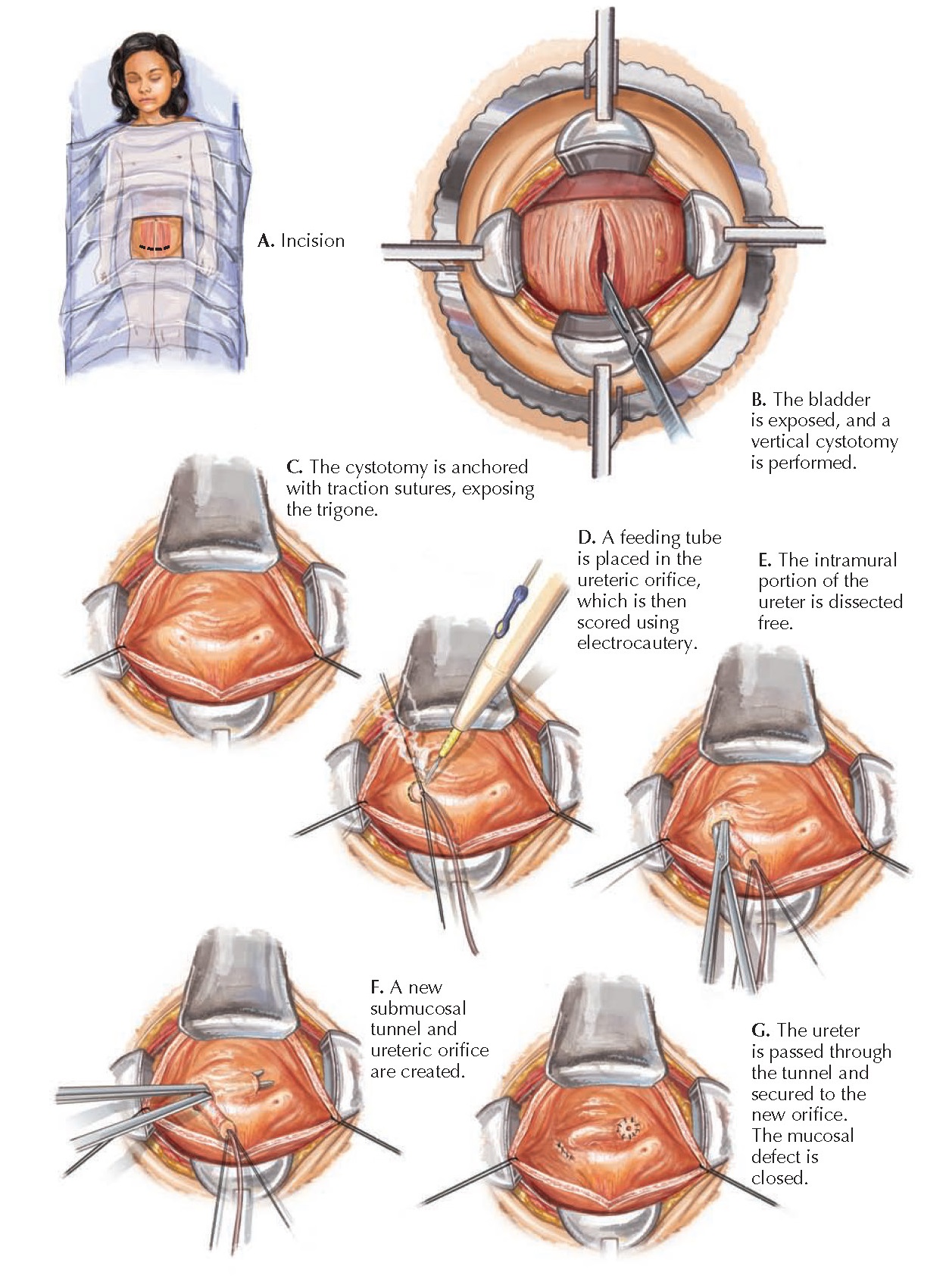
URETERAL REIMPLANTATION
There are several invasive strategies for the management of high-grade vesicoureteral reflux (VUR, see Plate 2-21), and the cross-trigonal ureteral reimplantation is one of the most popular and effective techniques. In this procedure, the refluxing ureter is dissected free of its attachments to the bladder wall, then advanced through a new submucosal tunnel that extends toward the opposite side of the trigone. The significantly lengthened intramural segment prevents further reflux. The surgery begins with a transverse incision approximately one fingerbreadth above the pubis to the lateral edges of both rectus muscles. The rectus fascia is incised transversely, and fascial flaps are raised. The rectus muscle bellies are longitudinally divided in the midline until the pubis is reached, then a self-retaining ring retractor is inserted to expose the bladder.
The
peritoneum is identified and avoided, and the bladder is opened from the dome to
just above the bladder neck. Traction sutures can be used to secure the
inferior aspects of the cystotomy to the rectus fascia. The self-retaining ring
retractor is repositioned to achieve a clear view of the trigone and ureteric
orifices. Rolled moist gauzes are counted and placed into the dome of the
bladder.
 |
| Plate 10-35 |
A 5-Fr
feeding tube is placed into the orifice of the refluxing ureter and then secured
using traction sutures at the 6- and 12-o’clock positions. The bladder mucosa
is scored around the orifice in an oval shape using needletip electrocautery
with a low cutting current. The plane of dissection is then established by
incising the bladder wall perpendicular to the ureter at the 6-o’clock position
of the orifice until the ureteral adventitia is reached. The intramural ureter
is then circumferentially dissected free of its attachments using fine tenotomy
scissors and a fine right angle clamp. In males, it is important to be cognizant
of the nearby vas deferens.
The traction
sutures and dissection sequentially release the intramural portion of the
ureter until an adequate length for reimplantation is obtained, usually defined
as four times the ureteral diameter. The dissection process often leaves a gap
in the detrusor floor, which should be reapproximated to prevent formation of a
diverticulum.
A new
submucosal tunnel is then established between the mucosa and detrusor. Tenotomy
scissors are introduced into the original hiatus (i.e., the site where the
ureter first enters the bladder wall) and advanced under the mucosa toward the
contralateral side of the trigone. Once a tunnel of adequate length has been
created, a new ureteric orifice is created by incising the mucosa. Using the
traction sutures to flatten the bladder floor facilitates this process.
The ureter
is passed through the new tunnel, with care taken to avoid twisting, and then
secured to the new orifice with a single stitch through the cuff of the distal
end of the ureter, the bladder mucosa, and the detrusor muscle. A feeding tube is
passed to confirm no twisting has occurred. The remainder of the cuff is sutured
to the bladder mucosa with interrupted absorbable sutures. The gap in the
bladder mucosa from the prior dissection is now closed with a running
absorbable suture. The feeding tube is passed a final time to ensure patency.
Stenting is not performed unless the ureter has been tapered (i.e., redundant
ureteral wall has been removed because the ureter was severely dilated).
The gauzes
are removed and counted, then the bladder is closed in two layers. The first is
an absorbable running suture of the bladder mucosa, followed by a running absorbable
suture of the seromuscular layer. The bladder is distended with saline through
a Foley catheter to confirm a watertight closure. The rectus muscles are then
reapproximated and the rectus fascia closed. The remaining fascial planes and
skin are then closed.
Postoperatively,
the patient should receive double the maintenance intravenous fluid rate for the
first 12 to 24 hours, which will irrigate the bladder and ureteral anastomosis. The Foley
catheter should remain in place for the first several days to facilitate healing
of the cystotomy. After the catheter is removed, the patient should void
frequently to maintain low bladder pressure. The routine use of postoperative
VCUG to check for resolution of reflux has been abandoned. An ultra-sound,
however, should be obtained several weeks after the surgery to assess for
possible hydronephrosis
secondary to ongoing ureteral obstruction.




