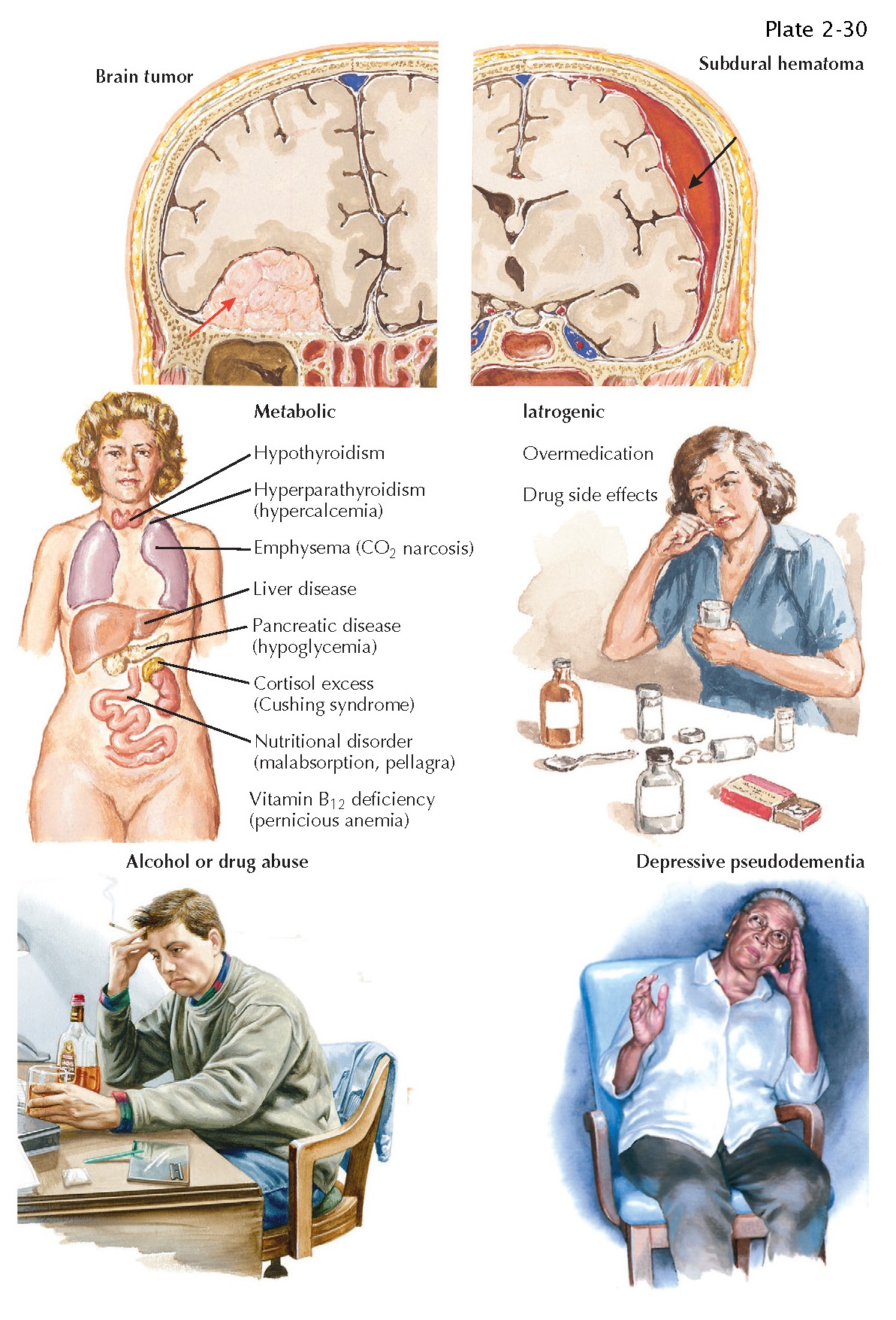
TREATABLE DEMENTIAS
Although in some ways cognitive performance abilities evolve throughout adulthood, many elderly people remain mentally sharp into their ninth and tenth decades. The emergence of uncharacteristic changes in an individual’s cognition that impacts their usual activities should, therefore, trigger an evaluation for possible etiologies.
Because Alzheimer disease is the
most common cause of intellectual decline in later life, symptoms or signs that
are unusual in Alzheimer disease should particularly alert the physician to a
different diagnosis and the possibility of reversing the dementing process.
Such features include early age at onset; prominent headache; disturbances of
gait or incontinence early in the course of the illness; epileptic seizures;
fever; precipitous decline over a period of weeks or months; alteration of
consciousness, especially sleepiness, stupor or delirium; history of head
trauma; focal neurologic signs, such as lateralized visual, motor, or sensory
abnormalities; accompanying dysfunction of peripheral nerves characterized by
paresthesias and absent distal reflexes; and known systemic cancer, collagen
vascular disease, or endocrinopathy. The presence of any of these features
should dictate further evaluation and consideration of the following treatable
dementias.
Metabolic Disease with Encephalopathy. When intellectual decline is caused by systemic metabolic disease, there are usually four associated features: diminished alertness; asterixis; a global decrease in mental function, often with a flight of ideas; and variability of intellectual function during the day. The metabolic dysfunction can be either endogenous or exogenous. An endogenous abnormality indicates too much or too little of a substance or metabolite usually found in the body, such as calcium, sodium, thyroid hormone, sugar, and so forth, may be responsible.
Failure of the lungs, kidneys, or
liver is also in this category. Exogenous metabolic dysfunction is caused by a
deficiency of a dietary substance, such as vitamin B12 or nicotinic acid, or by
intoxication with a growing variety of agents, such as alcohol, barbiturates,
or narcotics.
Brain Tumors. Primary benign brain tumors, such as
meningiomas, that affect the olfactory grooves and frontal lobes decrease
mental function by pressing on brain tissue or by obstructing the ventricular
system. Malignant primary metastatic tumors can also cause intellectual decline,
usually with focal or multifocal signs and seizures.
Head Trauma. A history of head injury, sleepiness, and slight
lateralized weakness are clues, particularly to a subdural hematoma. The
physician should be aware of this possibility because many patients will have
for- gotten the inciting trauma by the time they seek medical attention.
Normal-Pressure Hydrocephalus.
In most patients, this
occult condition is unrecognized until the pathologic state causes overt
symptoms.
Infection. An altered mental state, usually with head- ache
and cerebrospinal fluid (CSF) pleocytosis, may be the first indication of
central nervous system (CNS) syphilis, tuberculosis, or fungal meningitis.
Depression. Depression is associated with measureable
declines in some aspects of memory and memory complaints are a frequent symptom
of depression. Depressive pseudodementia is a concept that arose to
characterize depression as a potential mimic of dementia. Depression should be
considered in patients with dementia,
although depression is often an early expression of Alzheimer neuropathologic
changes in the brain. Depression in Alzheimer patients contributes to greater
functional decline and should be treated aggressively.
Cerebrovascular Disease. Strokes can decimate the regions of the brain
that govern thought processes. When this occurs, motor and reflex abnormalities
usually parallel or exceed the degree of intellectual decline. Usually, the patient also has a history
of an abrupt decline, as well as hypertension and coronary or peripheral
vascular disease.
Diagnostic Studies. Screening of biochemical parameters, especially
the vitamin B12 level and thyroid, renal, liver, and lung function can be
important in evaluating potential causes of dementia. Neuroimaging,
electroen-cephalography, and CSF analysis
may also detect unsuspected causes of dementia.