STAPHYLOCOCCUS AUREUS SKIN INFECTIONS
Cutaneous infection with Staphylococcus aureus can manifest in many ways. With the emergence of methicillin-resistant S. aureus (MRSA), these cutaneous infections have once again been given the attention they deserve. Most cases of MRSA are community acquired, and they have entirely different sensitivity patterns than those of hospital-acquired MRSA infections. These cutaneous infections are increasing in incidence. They not only cause significant skin disease but have the potential to become systemic and cause septicemia, pneumonia, osteomyelitis, and other internal infections. S. aureus is a transient colonizer of the skin and nasopharynx. This bacteria has shown a remarkable ability to develop and acquire antibacterial resistance mechanisms. S. aureus and MRSA are major hospital-acquired S. aureus infections, and now community-acquired MRSA has become just as important. MRSA accounts for more than 50% of hospital-acquired S. aureus infections.
The
emergence of community-acquired MRSA has led to an increase in the number of
serious S. aureus infections. These community-acquired strains have been
shown to cause an increased incidence of skin furuncles and abscesses as well
as severe pneumonia. Most of these infections occur in young, previously healthy
individuals.
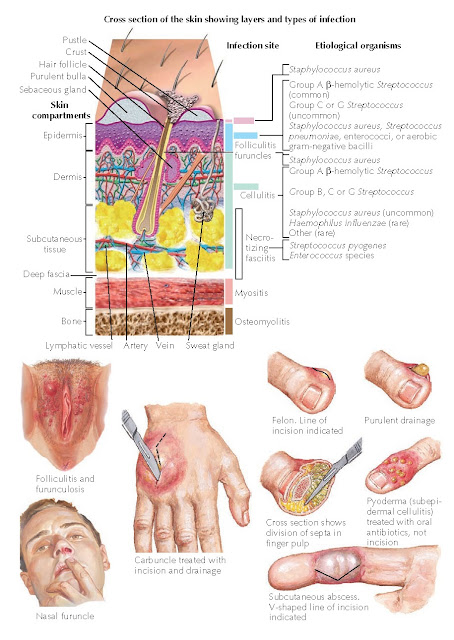 |
| Plate 6-25 TYPES OF SKIN INFECTIONS |
Clinical
Findings: S. aureus and MRSA can cause a wide range of cutaneous infections. The most
superficial of all infections that this bacteria causes is impetigo. Impetigo is often seen in children
and in people with preexisting skin diseases, which increase the likelihood of
cutaneous infections. The two most common causes of impetigo are S. aureus and
Streptococcus pyogenes or group A streptococcus. The disease often
manifests on the face. Regardless of the location, the infection appears as
small, superficial, honeycolored crusts with some weeping of yellow, clear
serum. There is a bullous variant, and it manifests with superficial blisters
that easily rupture. The disease is contagious and can be spread among
children. Typically, topical therapy yields excellent results, and oral therapy
can be avoided. If one were to biopsy a lesion of impetigo, a superficial
infectious process would be seen in the stratum corneum. Neutrophils and
bacterial elements would be found within the stratum corneum.
Infection of
the hair follicle shaft, termed folliculitis, can occur with a wide
variety of bacterial infections, including both S. aureus and
streptococcal species. Many other forms of folliculitis have been described
with other etiologic agents. Hot tub folliculitis is caused by Pseudomonas
aeruginosa, which grows in improperly disinfected hot tubs. Gram-negative
folliculitis can be seen in patients receiving long-term antibiotic therapy for
acne and other conditions. Regardless of the bacterial agent, the appearance of
folliculitis is the same. A small (1-3 mm) pustule is present and surrounds a
hair follicle. The pustule is easily broken and can be slightly itchy to
slightly painful. The hair can easily be removed from the pustule with minimal
effort. The pustule is surrounded by a millimeter or two of erythema, which in
turn is surrounded by a blanched region extending out another few millimeters.
Typically, entire regions of the body are affected, such as the legs or buttocks.
Folliculitis
can lead to furuncles (boils) or carbuncles (large furuncles). However, most
furuncles do not develop from a preexisting folliculitis. The furuncle is a
deep-seated, red, inflamed, tender nodule. Furuncles can occur in any location
and are commonly found within the nostril. The nostril is a location that S.
aureus is known to colonize. Furuncles may become quite large and
spontaneously drain to the surface. Before the drainage occurs, one can often appreciate the presence
of a pustule developing within the central portion of the furuncle. Carbuncles
appear to result from the coalescence of multiple furuncles. They can be large
and can have multiple draining sinus tracts to the surface of the epidermis.
Multiple pustules may precede the drainage. Pain and localized adenopathy are hallmarks of
both furuncles and
carbuncles.
Cellulitis
develops from a bacterial infection within the dermis or the subcutaneous fat
of the skin. The most frequent location is on the lower extremities. It occurs
more commonly in people with diabetes, trauma to the skin, poor vascular
circulation, or immunosuppression. Cellulitis starts as a small, pink-to-red
macule that slowly expands and can encompass large portions of the skin. This
is associated with edema and pain. The condition is almost always unilateral.
The pain can be severe. Tender adenopathy of regional lymph nodes is present.
Fever and systemic symptoms are almost always present. The redness is able to
travel many centimeters a day. The presence of red lines is more indicative of
a lymph- adenitis than a cellulitis, but these conditions can coexist.
Erysipelas is a more superficial form of cellulitis that occurs in the upper
dermis. It manifests clinically as a well-demarcated, edematous red macule that
is tender to the touch. The lower extremities and the face are common areas of
involvement.
Toxic
shock syndrome (TSS) is the name given to the development of fever, hypotension, and
nearerythroderma. The rash can appear as widespread, red, blanching macules. If
appropriately treated, the rash causes desquamation of the skin and return to
normal within a few weeks. TSS was initially reported after the use of
superabsorbent tampons, which were left in place for the entire menstrual
cycle. These tampons are no longer available. The superabsorbent tampons
provided an environment conducive to the rapid growth of S. aureus.
Toxins produced by the bacteria are responsible for the symptoms. TSS can occur
after any S. aureus infection but is much more likely with an abscess.
The toxins act as superantigens and activate T cells without the normal immune
system processing. This can lead to massive activation of the immune system.
Pathogenesis:
S.
aureus is
a gram-positive bacteria that is found throughout the environment and can be a
colonizer of humans. It is most likely to be found colonizing the nares, the
toe web spaces, and the umbilicus. The bacteria grows in grape-like clusters on
blood agar cultures. S. aureus is one of the most common bacterial
causes of human infection.
Histology:
The
histological findings are based on the form of infection biopsied. The common
underlying theme is a neutrophilic infiltrate that can be present throughout
the biopsy specimen. Bacteria are present and can be highlighted on tissue Gram
staining. The inflammation in impetigo is often limited to the epidermis, with
bacteria and neutrophils present within the stratum corneum. Superficial
blistering may occur within the granular cell layer in bullous impetigo.
Folliculitis shows edema and a neutrophilic infiltrate in and around the hair
follicle. Furuncles, carbuncles, and abscess show a massive dermal infiltrate
with neutrophils and bacterial debris.
The
pathology of cellulitis is more subtle, with neutrophils around blood vessels.
Bacteria can be difficult to see or to culture from skin biopsies of
cellulitis. Most cases of cellulitis are not biopsied. TSS shows a superficial
and deep mixed inflammatory infiltrate. No bacteria are seen, because the rash
is toxin mediated.
 |
| Plate 6-26 TOXIC SHOCK SYNDROME |
Treatment:
Impetigo
can be treated with topical therapy against S. aureus and streptococcal
species. Mupirocin is one such
topical agent that is highly effective. The other forms of infection need to be
treated with oral antibiotics. Cephalexin or dicloxacillin is a good first
choice. In areas with high rates of community-acquired MRSA, one should
consider covering for this agent with a sulfa-based medication or a
tetracycline derivative in adults. Culturing of the bacterial agent should be
done in all cases to select the most effective medication.
Severe cases
of cellulitis and all cases of TSS should be treated in the hospital in the
appropriate setting. Intravenous antibiotics are always used, and vancomycin is
the initial choice until the strain of S. aureus is isolated and
sensitivities are assessed. Once the sensitivities of the bacteria have been
determined, the antibiotic treatment can be tailored to the individual patient.
Patients with TSS often require intensive care with pressure support and respiratory support.




