SIMPLE AND RADICAL NEPHRECTOMY
Simple nephrectomy refers to the surgical removal of the kidney without the renal fascia or ipsilateral adrenal gland. This technique may be employed to treat non-neoplastic, irreversible kidney disease that poses an ongoing threat to the patient’s health. Possible indications include chronic pyelonephritis, chronic renal obstruction, extensive untreated nephrolithiasis, trauma, and ischemic nephropathy secondary to renal artery stenosis.
Radical
nephrectomy, meanwhile, refers to the surgical removal of the kidney along with
the perinephric fat, renal fascia, ipsilateral suprarenal gland, and ipsilateral
retroperitoneal lymph nodes. Radical nephrectomy is the treatment of choice for
patients with renal malignancies.
Both simple
and radical nephrectomy may be performed using either an open or laparoscopic
technique. In many cases, the surgeon will approach a simple nephrectomy with
the same surgical strategy as a radical nephrectomy. Simple nephrectomies,
however, may be technically more difficult because of the tissue fibrosis that
commonly occurs secondary to chronic inflammation.
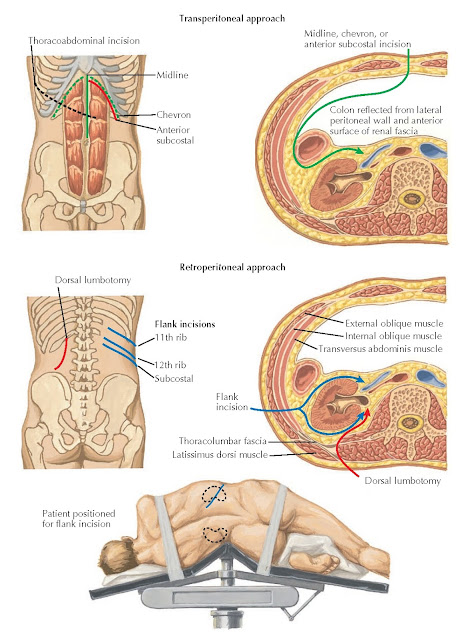
OPEN NEPHRECTOMY: INCISIONS FOR TRANSPERITONEAL AND RETROPERITONEAL APPROACHES
Plate 10-19
OPEN
TECHNIQUE
An open
nephrectomy may be performed from a trans-peritoneal or retroperitoneal
approach. Transperitoneal
Approach. The anterior subcostal and chevron incisions are the standard incisions
for the transperitoneal approach. For both, the patient is placed in supine
position, and an incision is made approximately two fingerbreadths below the
costal margin. The incision extends from the anterior axillary line either to
the xiphoid process (anterior subcostal incision) or to the opposite anterior
axillary line (chevron incision). The dissection is carried down through the
flank musculature (latissimus dorsi, external oblique, internal oblique,
transversus abdominis), anterior rectus fascia, and rectus abdominis muscles.
The round ligament of the liver (ligamentum teres) is clamped and ligated. The
colon is mobilized medially, and then the plane between the colonic mesentery and renal fascia is
developed. The renal hilum is approached anteriorly, and the vessels are
ligated using a combination of silk suture and surgical clips. The ureter is
identified and ligated. The upper pole of the kidney is separated from the
adrenal gland if desired.
A midline
transperitoneal incision may be used for patients undergoing exploratory
laparotomy for trauma, during which an indication for nephrectomy may be
discovered. It is not a common incision in planned surgeries on the kidney,
however, because the surgeon is often forced to operate caudal to the kidney.
Such an approach can make it difficult to achieve control of the hilar vessels,
especially in obese patients.
A
thoracoabdominal incision is used when radical nephrectomy is required in a
patient with a large, right- sided upper pole tumor. The main advantage to this
approach is the excellent exposure of the suprarenal area because inadequate
retraction of the liver from another approach could impede vascular control and
complicate removal of a large mass. The incision begins in the eighth or ninth
right intercostal space near the angle of the rib and is carried medially to
the midpoint of the left rectus muscle. The dissection is carried down to the
pleura and diaphragm, which are circumferentially incised to expose the liver.
The liver is then fully mobilized and retracted cephalad. Next, the duodenum is
mobilized medially to expose the kidney and hilum. After the kidney is removed,
the diaphragm must be sutured, a chest tube placed, and the pleura repaired.
This approach is associated with a considerable risk of injury to the lung, and
there is also significant postoperative morbidity associated with the use of a
chest tube. Therefore, this approach should be reserved only for large,
right-sided upper pole tumors that cannot be safely removed with an anterior
subcostal or chevron incision.
The major
advantages to transperitoneal open access include the excellent exposure to the
renal hilum and a large surgical field, whereas the disadvantages include the
risk of adjacent organ injury and of prolonged ileus.
Retroperitoneal
Approach. The flank incision is the standard incision for the retroperitoneal
approach. The patient is placed in the lateral position after induction of
anesthesia, with the table flexed at the level of the twelfth rib to maximize
the space between the costal margin and the iliac crest. An incision is made
directly over the eleventh or twelfth rib starting posteriorly at the lateral
edge of the erector spinae muscles. The rib chosen for dissection and possible
removal is the one nearest the hilum, which can be determined most accurately
on cross-sectional imaging. (The original method for making this determination
was to draw a horizontal line on an intravenous pyelogram from the hilum to the
most lateral rib the line intersects.) Dissection is carried through the
latissimus dorsi, external oblique, and internal oblique musculature to the
rib, which may be either retracted or resected. The transversus abdominis
muscle and tendon of origin, as well as the thoracolumbar and transversalis
fascia, are then incised to expose the paranephric fat. The peritoneum is
identified and swept medially with manual dissection to separate it from the
paranephric fat, which is then dissected to expose the renal fascia. In the
case of a simple nephrectomy,
the renal fascia is entered along its lateral surface. The kidney is pulled
laterally to reveal the renal vessels and ureter, which are ligated. The kidney
is then removed.
A dorsal
lumbotomy incision can be used when retroperitoneal access to the kidney is
desired in patients who have fibrosis associated with prior abdominal or flank
incisions. The incision is started over the erector spinae muscles at the level
of the twelfth rib, then continued downward and laterally toward the iliac
crest.
The
thoracolumbar fascia is incised lateral to the quadratus lumborum and erector
spinae muscles, which are retracted medially. The transversalis fascia is then
divided to expose the paranephric fat. An advantage of this approach is that it
avoids transection of the abdominal muscles; however, it provides limited
access to the hilum, making it difficult to control vascular complications.
The major
advantages of retroperitoneal open access include the avoidance of the
peritoneal space, which reduces the rate of
injury to intraabdominal organs and the risk of postoperative ileus. The major
disadvantage is that the renal vessels are not as easily visualized as in a
transperitoneal approach.

Plate 10-20
OPEN SIMPLE NEPHRECTOMY: FLANK APPROACH
LAPAROSCOPIC
TECHNIQUE
A
laparoscopic nephrectomy can also be performed from either a transperitoneal or
retroperitoneal approach.
With a
transperitoneal approach, the first step is to access the peritoneal cavity and
establish a pneumoperitoneum using a Veress needle or open Hasson technique.
After adequate insufflation of the abdomen, the first trocar is placed blindly
into the abdomen. The laparoscope is inserted and the abdominal contents
inspected for potential injury. Subsequent trocars are then inserted under
direct laparoscopic vision. The number and configuration of trocars vary
according to individual surgeon preference, but the basic principles of renal
triangulation should be observed. The colon is mobilized medially and released
of its attachments to the liver or spleen. The kidney is then retracted
laterally to facilitate identification of the ipsilateral psoas muscle, gonadal
vein, and ureter. The renal artery and vein are carefully dissected to
determine if there are accessory vessels or segmental vessel branches, then the
artery and any accessory branches are ligated using a laparoscopic surgical
stapling device. Additional dissection is performed to confidently eliminate all
bleeding from the arterial stump. The vein is targeted and ligated in the same
manner, then the ureter is divided. The upper pole of the kidney is separated
from the adrenal gland as needed. Finally, the kidney is placed in a
laparoscopic collection bag and removed through either an extension of a trocar
incision or through a separate skin incision (typically Pfannenstiel). The
pneumoperitoneum is reduced to ensure adequate hemostasis, and the trocar sites
are closed.
With a
retroperitoneal approach, the first step is to make a small incision over the
tip of the twelfth rib. A surgical clamp is then used to puncture the
thoracolumbar fascia and enter the retroperitoneum. Manual dissection is
performed to free additional space, and the psoas muscle is located using
tactile feedback. Next, a balloon trocar is placed in the space and inflated to
expand the surgical field. The space is then insufflated, and additional trocars
are inserted. The kidney is mobilized by separating the psoas muscle from the
paranephric fat and renal fascia. The renal hilum is then identified and divided, as noted
earlier.

Plate 10-21
LAPAROSCOPIC RADICAL NEPHRECTOMY: TRANSPERITONEAL APPROACH (LEFT-SIDED)
COMPLICATIONS
The
complications associated with nephrectomy include standard surgical
complications, such as bleeding, infection, wound separation, myocardial
infarction, cerebral vascular accident, deep vein thrombosis, pulmonary
embolus, cardiac dysrhythmia, ileus, and atelectasis. In addition, several
complications are specific to this procedure, including renal insufficiency and
injury to adjacent organs
(perforation of bowel, disruption of retroperitoneal vasculature, pancreatic
ductal injury/ fistula formation, pneumothorax).
Laparoscopic
approaches in particular can be complicated by visceral or vascular injuries during
initial access with the Veress needle or trocars. In addition, patients should
always be warned that all laparoscopic cases have the potential for conversion
to an open procedure.




