POTASSIUM-SPARING DIURETICS
ACTIONS AND MECHANISM
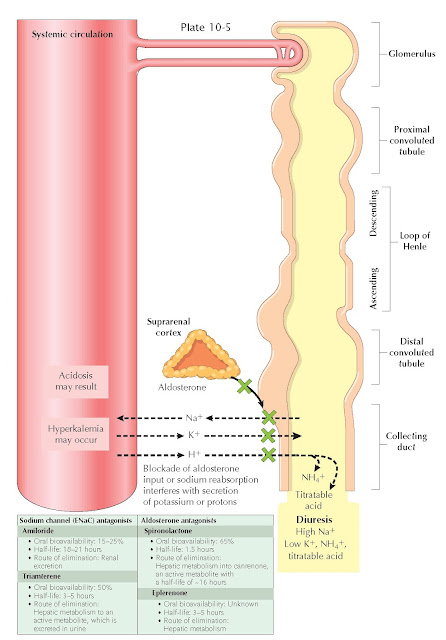
In the connecting tubule and cortical collecting duct, principal cells are responsible for K+ secretion through two major mechanisms. First, the reabsorption of Na+ through apical ENaC channels leaves a negative charge in the tubular lumen, which promotes the secretion of potassium through apical ROM-K channels. Second, increased flow rates through the distal nephron stimulate K+ secretion through apical maxi-K channels.
Most diuretics including carbonic anhydrase
inhibitors, loop diuretics, and thiazide diuretics up-regulate distal K+ secretion
through several mechanisms. First, these agents interfere with Na+ reabsorption
in more proximal portions of the nephron, which increases the load that reaches
the distal nephron. The increased Na+ gradient across the apical
surface of principal cells increases reabsorption through ENaC channels, which
then leads to increased K+ secretion through ROMK channels. Second,
these agents cause volume loss, which activates the
renin-angiotensin-aldosterone system. One of aldosterone’s effects is to
up-regulate ENaC channels, which increases Na+ reabsorption and, by
necessity, also increases K+ excretion. Finally, diuretics increase
urine fl ow rates through the distal nephron, which stimulates K+
secretion through apical maxi-K channels.
The “potassium-sparing”
diuretics interfere with sodium reabsorption across ENaC channels, which
produces a small diuretic effect and, more importantly, eliminates one of the
major causes of K+ secretion. This category of diuretics encompasses
two different classes of agents: those that directly block the ENaC channel
(amiloride and triamterene) and those that block aldosterone signaling (spironolactone and
eplerenone).
ENaC channel blockers
enter the nephron through the organic cation pathway in the proximal tubule.
Upon reaching principal cells, these agents bind to the ENaC channel from its
luminal side, competing with Na+ ions for negatively charged sites
in the pore. Meanwhile, aldosterone receptor blockers remain in the plasma to
act at the basolateral surface of principal cells.
Potassium-sparing
diuretics usually have only a small diuretic effect. Nonetheless, they can be
useful in combination with other classes of diuretics because of their effects
on potassium homeostasis. They can also help offset the increase in distal
sodium reabsorption that occurs with the use of other diuretics.
COMMON AGENTS
The major
potassium-sparing diuretics are listed in the plate.
INDICATIONS
The major indications for
potassium-sparing diuretics include:
• Hypokalemia,
especially if associated with the use of another diuretic
• Liddle
syndrome (ENaC blockers)
• Primary
hyperaldosteronism (aldosterone antagonists)
• Congestive
heart failure (aldosterone antagonists)
• Ascites
(aldosterone antagonists)
ADVERSE
EFFECTS
The major
adverse effects of potassium-sparing diuretics include:
• Hyperkalemia
• Metabolic
acidosis. Through the same mechanisms used to reduce K+ secretion, these agents also reduce H+ secretion
into the distal nephron.
• Acute
kidney injury (triamterene, owing to crystalluria and tubular obstruction)
• Nausea,
vomiting, and diarrhea
• Peptic
ulcers (spironolactone)
• Headache
and lethargy
• Rash
• Antiandrogenic
effects: gynecomastia and/or breast pain, impotence, hirsutism, and irregular menses (aldosterone
antagonists, spironolactone more than eplerenone)