IMPLANTATION AND
EARLY DEVELOPMENT OF OVUM
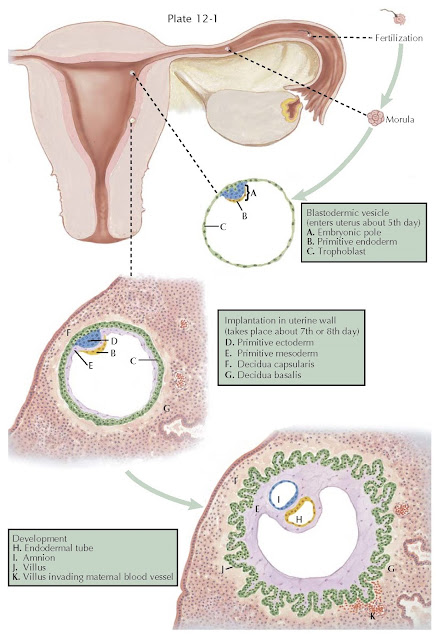
Fertilization of the human ovum usually occurs in the ampullary portion of the oviduct, although in rare instances it may take place elsewhere in the genital tract or even in the ovary. Soon after the spermatozoon enters the ovum, the male and female pronuclei fuse to form the segmentation nucleus, which rapidly divides and redivides. Segmentation, thus initiated, continues until the original fertilized ovum is transformed into a mass of cells called the morula.
At this early stage, two types of
cells can be distinguished; some proliferate more rapidly, forming a sphere
that encloses the aggregate of more slowly dividing cells. A semifluid substance
is excreted from the outer cells and is collected in a cavity, which forms
simultaneously. The sphere-shaped structure is called the blastodermic vesicle
or blastocyst. One layer of ectodermal cells, the primitive trophoblast, covers
it except at one pole where the rapidly dividing cells have formed the “inner cell
mass,” which constitutes the beginning of the embryo.
While these changes take place, the
ovum continues its passage into the uterine cavity, where it becomes implanted
on the seventh or eighth day after ovulation. Various conditions may slow or
obstruct the passage and cause nidation elsewhere, resulting in an ectopic
pregnancy.
If the zygote splits very early
(first 2 days after fertilization), each cell may develop separately its own
placenta (chorion) and amnion (dichorionic diamniotic twins), which occurs 18%
to 36% of the time. Most of the time, in monozygotic twins the zygote will
split after 2 days, resulting in a shared placenta but two separate sacs
(monochorionic diamniotic twins), occurring 60% to 70% of the time. In about 1%
to 2% of monozygotic twinning the splitting occurs late enough to result in
both a shared placenta and a shared sac (mono-chorionic monoamniotic twins).
Later splitting of the zygote may result in conjoined twins.
During the menstrual cycle, the
ovarian hormones, estrogen and progesterone, act upon the endometrium,
producing the premenstrual mucosa, which is sloughed or cast off during menstruation but remains when
fertilization occurs. The pregravid endometrium gradually undergoes further
changes to become the early decidua to which the blastocyst rapidly adheres
once it has reached the uterus.
By the invasive capacity of its
trophoblastic cells, the blastocyst sinks into the endometrium, which then
closes over it and seals it from the uterine cavity, forming the decidua
capsularis. The remaining decidua surrounding the blastocyst is called the
decidua basalis, whereas the term decidua vera or parietalis designates
the entire endometrium lining the uterus, except for the parts surrounding the
blastocyst.
During the period of migration and
implantation of the blastocyst, marked cellular proliferation has been taking
place in the embryonic area. Three types of cells can be differentiated within
the “inner cell mass.” These constitute the three primary germ layers, the ectoderm,
endoderm, and mesoderm.
From the ectoderm will derive the
central nervous system, the epidermis, and certain skin appendages.
The endoderm will furnish the
epithelial linings and the glands of the gastroenteric and respiratory tracts.
The mesoderm will give rise to the epithelium of the urinary and genital
systems, the linings of the serous cavities, the various supporting tissues of
the body, the blood, and the cardiovascular system.
After implantation, mesodermic cells
grow out beneath the primitive trophoblast, which, by proliferation, forms
villous projections into the surrounding decidua.
Each villus consists of a mesodermic core covered by two layers of
trophoblastic cells. The outer cells have dark-staining nuclei and indefinite
cell out-lines. They are called syncytial trophoblasts. The more distinct cells
of the inner layer are designated cytotrophoblasts or Langherans cells. These
decrease in number as pregnancy progresses and are difficult to find after the third month of gestation.