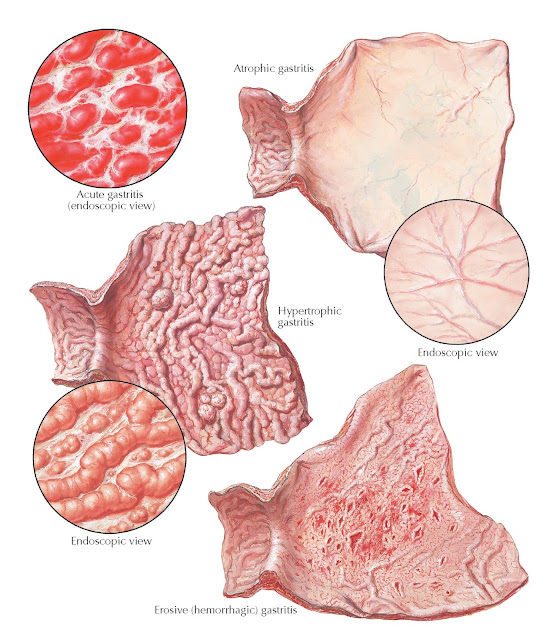
GASTRITIS
Gastritis is an inflammation of the mucosal lining of the stomach. It can occur suddenly (acute) or gradually (chronic). Gastritis can be caused by irritation or inflammation from excessive alcohol use or the use of certain medications such as aspirin or other anti inflammatory drugs. It may also be caused by H. pylori and other bacterial and viral infections, pernicious anemia, and bile reflux.
Gastric irritation from abuse of
alcohol, coffee, and tobacco and from chemicals and drugs such as NSAIDs and,
perhaps, corticosteroids is the main cause of acute gastritis. Acute
gastritis may also develop during many febrile infections, such as typhoid,
pneumonia, and diphtheria. H. pylori infection can present with acute
gastritis. The gastric mucosa in acute gastritis is erythematous, often with
erosions, and may be covered with a thick mucus. Symptoms of gastritis vary
among individuals, and in many people there are no symptoms. The most common
symptoms include epigastric pain or discomfort, nausea or indigestion,
vomiting, a burning or gnawing feeling in the stomach between meals or at
night, and a disagreeable taste. A corrosive type of gastritis, originating
from the intake of strong chemicals such as lye, can lead to a localized or diffuse
necrosis and permanent scarring.
 |
| Plate 4-42 |
Erosive hemorrhagic gastritis is characterized by multiple, diffuse erosions
in an inflamed mucosa. Nausea, anorexia, pain, and gastric hemorrhage may
occur. This acquires a special clinical significance with its tendency to cause
severe, at times life-endangering, hemorrhages. Larger arteries extend quite
frequently as far up as the epithelium and may become involved in some of the
many small, but by no means superficial, erosions. Whenever the origin of
gastrointestinal bleeding cannot be identified, the possibility of an erosive
hemorrhagic gastritis must be seriously considered, especially in severely ill
hospitalized patients. Endoscopy is important for the diagnosis, though during
an episode of acute bleeding the mucosa may not be well visualized. At
laparotomy the diagnosis may still be difficult, because, even when viewing the
mucosa directly after gastrostomy, the small erosions (i.e., the source of the
bleeding) may not be well seen macroscopically.
A similar type of hemorrhagic
gastritis has been observed after partial resection of the stomach
or after gastroenterostomy or ulcer. This should be kept in mind if the
suspicion of a bleeding peptic “anastomotic ulcer” cannot be confirmed
unequivocally by x-ray studies, endoscopically, or at laparotomy. Under such
circumstances, vagotomy may be the best procedure to stop the bleeding. It has
helped in many cases and, in any event, is preferable to an additional
resection.
Chronic atrophic gastritis is a process of chronic inflammation of the
stomach mucosa, leading to loss of gastric glandular cells and their eventual
replacement by intestinal and fibrous tissues. This may be an aftermath of an
acute gastritis, but many other possible etiologic factors of exogenous or
endogenous origin need to be considered. Chronic atrophic gastritis has a close
relationship to pernicious anemia and vitamin B12 deficiency. The relationship
of chronic atrophic gastritis and, more specifically, pernicious anemia with
malignancies has not been clarified. The characteristic features of chronic
atrophic gastritis endoscopically are the disappearance of the folds and the
thinness of the mucosa through which shines the vascular net, both arterial and
venous. Microscopically, the chief and parietal cells are considerably reduced
in size and number; the epithelial cells are transformed to a great extent into
goblet cells, or undergo metaplastic changes. The clinical manifestations are
rather nonspecific. Upper endoscopy with biopsies of the gastric body is used
to establish the diagnosis.
With chronic hypertrophic
gastritis the situation is clinically much the same, except that
hyperacidity is present in most cases, and the distribution of the rugae and
the “cobblestone” appearance of the mucosal surface, seen roentgenographically,
provide more often the right clue for diagnosis; endoscopy is needed to make
the unequivocal diagnosis. The rugae are strikingly thickened and, even at
autopsy, do not flatten out when the wall is stretched. Ménétrier disease (also
known as hypoproteinemic hypertrophic gastropathy) is a rare, acquired disorder
of the stomach characterized by greatly thickened gastric folds and excessive
mucus production, with resultant protein loss leading to diarrhea. Other
conditions, such as lymphoma and Zollinger-Ellison syndrome, can cause
hypertrophic mucosal folds in the stomach, and use of proton pump inhibitors
can also be a cause. In Zollinger-Ellison syndrome, or gastrinoma, the elevated
serum gastrin levels lead to parietal cell hypertrophy, prominently in the
fundus and body of the stomach. The use of proton pump inhibitors results in
gastric hypoacidity leading to increases in gastrin levels and, also, parietal
cell hypertrophy.




