FUNCTIONAL DYSPEPSIA
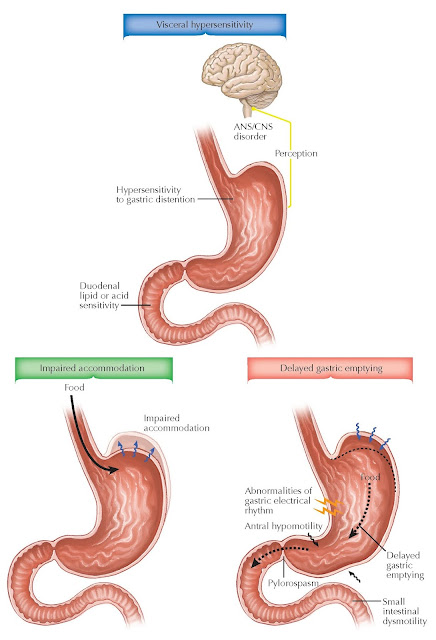
Dyspepsia refers to symptoms originating in the upper gastrointestinal tract; the term is used to describe upper abdominal pain or discomfort, early satiety, and postprandial abdominal bloating or distention. Some examples of structural or biochemical disorders causing dyspepsia include gastroduodenal ulcer, gastritis, GERD, and gastric cancers; medication side effects may also be a cause. In many patients, the cause of dyspepsia is idiopathic and not obvious after an evaluation including the history, a physical examination, blood work, and upper endoscopy; this is termed functional dyspepsia. ROME criteria for functional dyspepsia developed to help describe these particular patients include the following requirements: (1) the presence of one or more of the following: bothersome postprandial fullness, early satiation, epigastric pain, or epigastric burning; and (2) no evidence of structural disease (including at upper endoscopy) that is likely to explain the symptoms. Functional dyspepsia in the ROME classification is divided into (1) postprandial distress syndrome characterized primarily by early satiation and postprandial fullness; and (2) epigastric pain syndrome characterized primarily by epigastric pain and burning. Several mechanisms have been proposed for the pathogenesis of functional dyspepsia. The gastric acid or inflammation hypothesis suggests that gastric acid or inflammation from gastric acid, bile, GERD, or H. pylori infection is responsible for symptoms. The motor disorder hypothesis suggests that gastric motility disorders, such as gastroparesis, impaired fundic accommodation, antral distention, or gastric dysrhythmias, are important. The visceral hypersensitivity hypothesis proposes exaggerated symptoms in response to physicochemical stimuli, such as distention, contraction, acid, and bile. The psychological hypothesis suggests that some of the symptoms are related to or enhanced with depression, anxiety, or a somatization disorder.
There are
several pathophysiologic alterations of gastric motility and sensation in
functional dyspepsia. Delayed gastric emptying, impaired gastric accommodation
to a meal, and visceral hypersensitivity are important pathophysiologic factors
in functional dyspepsia. One or more of these factors may be detected in two
thirds of patients with the disorder.
 |
| Plate 4-50 |
Delayed
gastric emptying is present in approximately a third of patients with
functional dyspepsia. It has been suggested that the severity of postprandial
fullness and vomiting is correlated with delayed gastric emptying, although
some studies could not confirm this. Functional dyspepsia patients with delayed
gastric emptying may respond better to prokinetic agents than patients with
normal emptying. The role of prokinetic agents in improving gastric emptying
and symptoms is inconsistent, however.
Regional
gastric function abnormalities may be present in many dyspeptic patients and
appear to correlate with dyspeptic symptoms. Normally, the stomach accommodates
to a meal by relaxation of the gastric fundus and corpus, providing the meal
with a reservoir and enabling a volume increase without a rise in intragastric
pressure. Impaired fundic accommodation has been found in a third of patients
with functional dyspepsia. Impaired proximal gastric accommodation was
associated with early satiety and subsequent weight loss. In research studies,
impaired fundic accommodation can be assessed using a gastric barostat,
scintigraphy, ultrasonography,
radionuclide imaging of the gastric wall with single-photon emission computed
tomography, or satiety testing with consumption of water or a liquid nutrient
drink.
Visceral
hypersensitivity or augmentation of visceral afferent sensation (nociception)
may be a major cause of symptoms in functional dyspepsia. A third of patients
have increased sensation to gastric and small intestinal distention. When the
stomach is stimulated by increasing volumes or increasing intragastric
pressures, patients experience symptoms at volumes that physiologically normal
subjects do not (allodynia), and they have more pain at levels when the
physiologically normal subjects begin to have pain (hyperalgesia). The
symptoms may result from an exaggerated visceral sensory perception of normal
physiologic events. Brain activation by visceral stimulation with gastric
distention is being studied in functional dyspepsia using positron emission
tomography and functional magnetic resonance imaging. Patients with functional
dyspepsia may have abnormal activation of the cortical and subcortical sites in response to
gastric distention.




