DYSPLASTIC ACETABULUM AND PROTRUSIO
ACETABULI
Reconstruction of the dysplastic or deficient acetabulum presents a particularly difficult surgical challenge, because the anatomic landmarks commonly used as reference points may not be in their normal positions. Portions of the bony circumference of the acetabulum may be deficient as a result of old fractures or congenital dysplasia. For example, in a long-standing posterior fracture dislocation of the hip, the posterior wall of the acetabulum is usually severely deficient; in congenital dislocation of the hip, the acetabulum is shallow and poorly developed. If the femoral head has been dislocated for many years, it articulates with the iliac wing in a pseudoacetabulum. The true acetabulum is stunted, small, and shallow, but its anatomic configuration is usually preserved and identifiable once the contracted overlying inferior capsule is reflected.
DYSPLASTIC ACETABULUM
Dysplasia of the acetabulum is often seen without actual dislocation of
the femoral head. Usually, the acetabulum is shallow and the femur is displaced
laterally. The superolateral wall, or roof, of the acetabulum is deficient and
must be reconstructed with a bone graft before it can support an acetabular
prosthetic component.
Total hip replacement in the patient with congenital hip dislocation is
extremely difficult. Because the acetabulum may be deficient in bone mass and
the proximal femur malformed, as is common, modular prostheses are sometimes
required.
Treatment. A bone graft is often used to reinforce
the superior acetabulum; it can be fashioned from the resected femoral head.
The bone graft is fixed to the ilium with screws and then reamed to receive a small
acetabular component, with the pubic bone and ischium used as anterior and
posterior landmarks to avoid excessive reaming. Modular femoral components with
varying angles and neck lengths can be used to achieve a near-normal abductor
lever arm.
After a failed total hip replacement, bone autografts or allografts may
also be used to reconstruct an acetabulum that is
deficient in bone mass. After thorough removal of the loose acetabular
component, bone mass deficiencies are repaired. A new acetabular com- ponent,
often made with trabecular metal, is then impacted and secured with screws.
Segmental defects are preferably reconstructed with trabecular metal augments.
Cavitational defects, on the other hand, may be filled with allografts, usually
best impacted into the cavity in the form of chips. A smooth surface can be
created by reaming in reverse.
MEDIAL WALL DEFECT
Another common site of bone mass deficiency is the medial wall, or
floor, of the acetabulum. Often discovered during revision surgery, this
problem is frequently related to the first procedure, during which the medial
wall was perforated. This condition is also seen in inflammatory arthritis.
Treatment. Medial wall deficits have been classified
by size into three types: minor (diameter < 1 cm); intermediate (diameter < 3 cm); and major (diameter
> 3 cm). All deficits are repaired surgically with one of three types of
bone grafts. Bulk bone is used to recon- struct major deficits. For
example, a large plug is fashioned from a resected femoral head and used to
fill a medial wall defect. Screws may be added to further stabilize the graft,
and a hemispheric depression can be reamed in the graft. Chips of trabecular
bone are harvested and used as packing material to fill small deficits, cysts,
and cracks. Pulverized bone (from reaming or a bone mill) can be made
into a soft, pastelike consistency and finger packed into small deficits.
Bulky pieces of bone allograft maintain their structural integrity and
may be variously replaced by host living bone through a process called creeping
substitution; the trabeculae in the bone allograft act as a “trellis” for
the ingrowth of live bone. Cementing into a bone graft is possible as long as
the host bone–bone graft interface is adequate and intimate.
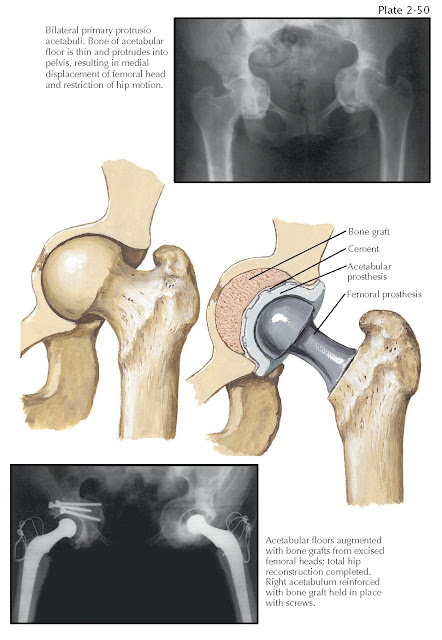
PROTRUSIO ACETABULI
As a result of any disease that causes bone resorption, the pelvic bones
become osteoporotic and soft and the medial wall of the acetabulum may be
gradually displaced medially. Bone remodeling in response to applied load
causes varying degrees of superomedial protrusion of the femoral head (see Plate 2-50). Protrusio
acetabuli occurs when the femoral head is displaced past the ilioischial line
in the pelvis. Other conditions that can cause progressive protrusion of the
acetabulum are osteomalacia, rickets, Paget disease of bone, and infections.
Central dislocation of the femur due to trauma can also heal with a protrusion
deformity. Arthrokatadysis (Otto pelvis) is a rare idiopathic form of severe
bilateral protrusio acetabuli most often seen in adolescent females. Metastatic
carcinoma to the pelvis can lead to pathologic fractures, which result in a
protrusion deformity.
 |
| PROTRUSIO ACETABULI |
Primary manifestations of protrusio acetabuli are thigh pain and
decreased range of motion. Lateral and rotatory movements are particularly
inhibited by the impingement of the femoral neck against the acetabular labrum,
or rim. A classification of protrusion deformities distinguishes cases with an
intact medial wall from those with a perforated medial wall. Third-degree protrusio
acetabuli is the most severe, occurring when the medial displacement is greater
than 5 mm, and is coupled with penetration of the medial wall. Protrusio
acetabuli prosthetica occurs when a hip prosthesis is gradually displaced
through the soft bone of the medial wall.
Treatment. Like medial wall defects, protrusio
acetabuli is treated with various types of bone grafts to reinforce areas
deficient in bone mass to ensure that prosthetic
components remain in the correct anatomic positions.
If there is enough anterior and posterior wall remaining, a cementless
socket is impacted in place with cancellous bone graft behind it. If severe
deficiencies are present, an antiprotrusio cage may be placed over the top of
the cementless socket. This cage rests on the ilium and ischium, thereby
transferring the load from the hip to the intact
pelvis.





