HEREDITARY BREAST
DISEASE
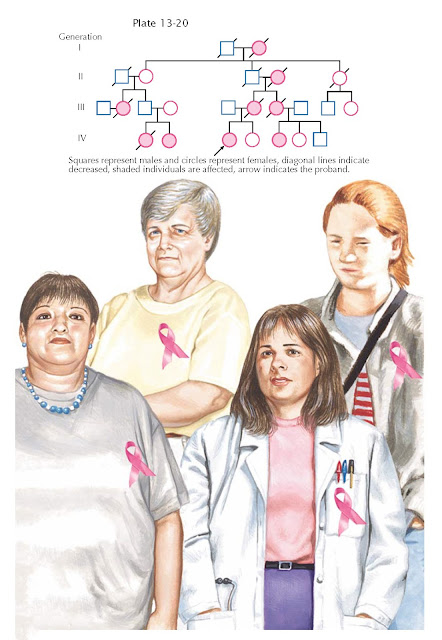
Approximately 5% to 10% of breast cancers have a familial or genetic link. In these families, breast cancer tends to occur at a younger age and there is a higher prevalence of bilateral disease. The association between inherited breast and ovarian cancer has lead to the term hereditary breast ovarian cancer syndrome (HBOC).
Hereditary breast ovarian cancer
syndrome is characterized by an early age of onset of breast cancer (often
before age 50). In affected families, there is a family history of both breast
and ovarian cancer and an increased chance of bilateral cancers or an
individual with both breast and ovarian cancer. Pedigrees will demonstrate an
autosomal dominant pattern of inheritance (vertical transmission through either
the mother’s or father’s side of the family). Members of these families also
have an increased incidence of tumors of other organs, such as the fallopian
tube or prostate. Families with cases of male breast cancer and families of
Ashkenazi Jewish ancestry are at increased risk for this syndrome (greater than
10-fold increase).
At least two genes have been found
in which mutations can cause this pattern of inherited breast and/or ovarian
cancer. It appears that germline mutations of the BRCA1 tumor suppressor gene
on chromosome 17q are responsible for a large proportion of these hereditary
cancers. However, not all families in which hereditary breast or ovarian cancer
is suspected are found to have mutations in either BRCA1 or BRCA2.
Having a single mutation in one of these genes does not appear to be sufficient
to have a tumor develop. It is generally thought that mutations in both
alleles, due to chemical, physical, or biologic environmental expo- sures, or
chance errors in cell replication, must occur for tumor development. To date,
hundreds of unique mutations have been identified in both BRCA1 and BRCA2,
most due to sporadic mutations unique to the individual or family. Specific
recurring mutations have been found in individuals of Ashkenazi Jewish descent
and persons from the Netherlands, Iceland, and Sweden. Mutations in the BRCA
family of genes confer a lifetime risk of breast cancer that approaches
85%, though the risk of ovarian cancer is variable depending on the location of
the mutation. The average lifetime risk of ovarian cancer is approximately 40%
to 50%.
The BRCA2 gene resides on
chromosome 13, and the DNA sequence was determined in 1995. A woman with a BRCA2
gene mutation also has an 85% lifetime risk of breast cancer and a 15% to
20% lifetime risk of ovarian cancer. This mutation is associated with male
breast cancer, conferring a 5% to 10% lifetime risk for a male with the
mutation. BRCA3 gene has been recently mapped to chromosome 8, but the
details of any associated clinical syndrome have not yet
been determined.
Presently, management
recommendations for women with BRCA mutations vary from earlier and
increased interval screening tests to prophylactic measures such as
chemoprevention with tamoxifen, mastectomy, and oophorectomy. A task force has
recommended breast self-examination beginning by age 20, annual or semi-annual
clinical examination beginning at ages 25 to 35 years, and annual mammograms
beginning at ages 25 to 35 years. They made no
recommendation for or against prophylactic surgery in these patients. Although
there is good evidence suggesting that tamoxifen can significantly reduce the
risk of breast cancer in women at high risk, there are still no conclusive data
on the use of tamoxifen in a population of patients with a BRCA gene
mutation. There are currently no effective screening techniques for the early
detection of ovarian cancer. For this reason, some women at high risk choose to undergo prophylactic oophorectomy.