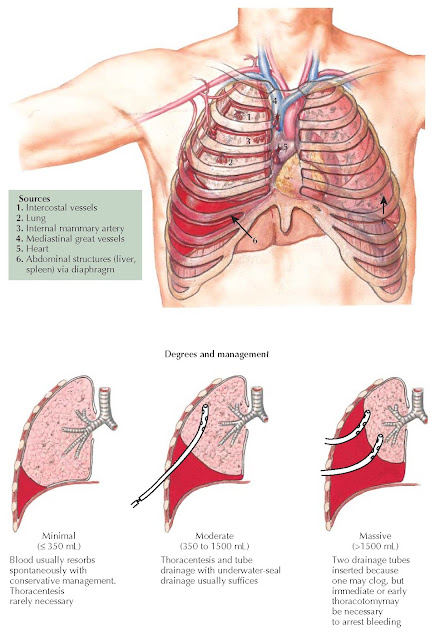
HEMOTHORAX
Hemothorax is bleeding into the pleural cavity; the source of bleeding can be from a variety of structures in the thorax or from the abdomen through a diaphragmatic injury. The most common cause of hemothorax after blunt trauma is the chest wall with disrupted parietal pleural allowing blood loss from torn intercostal vessels to enter the pleural cavity; after penetrating injuries, it is usually from the lung parenchyma. Persistent bleeding into the thorax suggests a systemic source, usually an intercostal or internal mammary artery, but occasionally a named thoracic vein (e.g., azygos, subclavian, or pulmonary) will produce ongoing blood loss. Typically, a hemothorax from a ruptured thoracic aorta, pulmonary artery, or heart is extensive at the time of emergency department arrival. Of note, occasionally, the source of major persistent bleeding in the thorax originates from the liver or spleen via an associated diaphragmatic injury.
The diagnosis of hemothorax is usually established by
chest radiography or with the presumptive placement of a chest tube in a
patient arriving in hemorrhagic shock. Hemothorax is recognized more frequently
with computed tomography (CT) scanning because small collections are seen that
are not apparent on chest radiography. Management is dictated by the size of
the hemothorax and physiologic condition of the patient. In general,
hemothoraxes can be considered minimal if they are smaller than 350 mL,
moderate at 350 to 1500 mL, and massive above 1500 mL. Minimal hemothoraxes are
usually first identified by CT scanning and can be treated expectantly. Moderate
hemothoraxes warrant tube thoracostomy because this evacuates the blood
completely; reexpands the lung, which tamponades chest wall bleeding; and
permits monitoring of continued blood loss. A chest tube placed for moderate
bleeding should be relatively large (e.g., 28 Fr in women and 32 Fr in men).
 |
| Plate 4-139 |
The tube should be placed after ample chest wall
preparation and generous local anesthesia. An incision should be made in the
midclavicular line at a relatively superior location on the chest wall (i.e.,
the fifth intercostal space) to avoid injury to the liver or spleen caused by a
high-lying diaphragm. A gloved finger should be inserted into the pleural space
to ensure proper positioning, and the tube should be directed into the lung
apex with a blunt clamp. After it is in position, 20 cm H2O is applied to the
chest tube to evacuate the pleural cavity quickly. Finally, the tube should be
sutured securely to the chest wall to avoid dislodgement during patient
transport. Follow-up radiography is essential to ensure good tube placement and
complete removal of the hemothorax. The initial management of a massive
hemothorax is similar except that a large chest tube (i.e., 36 Fr) should be
used. If the follow-up chest radiograph does not show complete blood
evacuation, a second large-bore tube
should be inserted.
The decision for emergent thoracotomy is largely
determined by the patient’s response to tube thoracostomy in conjunction with
evidence of ongoing bleeding. In general, an initial return of more than 1500
mL or the failure to eliminate a hemothorax with two chest tubes, referred to
as a coked hemothorax, warrants exigent thoracotomy. There is also
general agreement that chest tube output greater than 250 mL/h for 3 successful
hours requires thoracic exploration, although video-assisted thoracoscopy (VATS) may be reasonable
in hemodynamically stable patients. Alternatively, angioembolization may be
appropriate if the suspected source of persistent bleeding is an intercostal
artery. If a patient fails to resorb a moderate hemothorax after 72 hours or if
there is a delayed hemothorax refractory to tube thoracostomy, VATS is a very
effective maneuver for definitive removal of the retained hemothorax.




