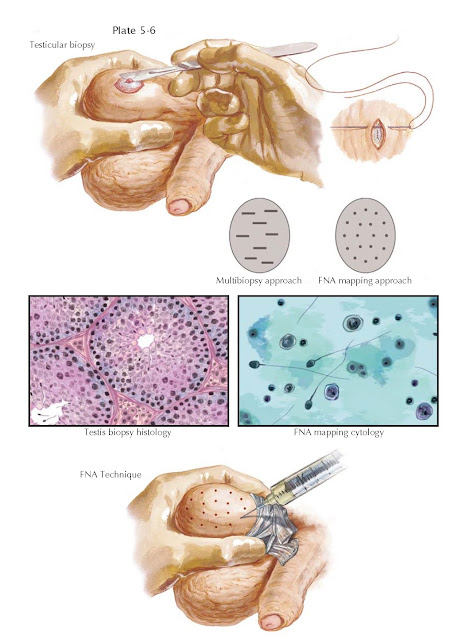
AZOOSPERMIA IV: DIAGNOSTIC PROCEDURES
The evaluation of the infertile, azoospermic man involves a direct assessment of spermatogenesis. This provides definitive evidence of either obstructive or nonobstructive azoospermia. The testis biopsy is most commonly used to assess sperm production. The technique involves a small, open incision in the scrotal wall and testis tunica albuginea under local anesthesia. A small wedge of testis tissue is removed, examined histologically, and seminiferous tubule architecture and cellular composition are assessed (for patterns, see Plate 3-21). Alternatively, percutaneous sampling of testis tissue with a biopsy gun can be used, similar to that employed for prostate biopsy. Although several excellent descriptions of testis seminiferous epithelium histology have been reported, no individual classification has been uniformly adopted as a standard approach.
A testis biopsy is not usually indicated for cases of oligospermia (low sperm
count), as partial reproductive tract obstruction is very rare. In addition,
although a single, unilateral testis will define excurrent ductal obstruction,
the finding of two asymmetric testes may warrant bilateral testis biopsies to
best define the pathology.
With normal sperm production, formal investigation of the reproductive
tract for obstruction is warranted, beginning with a vasogram (see Plate 5-5).
Abnormal sperm production defines the problem as nonobstructive azoospermia. The
testis biopsy may also indicate the premalignant condition, intratubular germ
cell neoplasia, that tends to occur globally within the affected testis. This
condition exists in 5% of men with a contralateral germ cell testis tumor and
is more prevalent in infertile than fertile men.
Since the advent of in vitro fertilization and intracytoplasmic sperm
injection (IVF-ICSI), a relatively recent indication for testis biopsy is to
determine whether or not men with nonobstructive azoospermia have mature sperm
present in the testis that may be used for assisted reproduction. A single
testis biopsy will detect the presence of sperm in 30% of men with
nonobstructive azoospermia. Other surgical and non- surgical approaches have
sought to improve the “yield” of sperm in cases of testis failure.
It is now clear that men with nonobstructive azoospermia can have
“patchy” or “focal” areas of sperm production in a testis otherwise devoid of
mature sperm. This has led to the development of more sophisticated approaches
to testis biopsy, including multibiopsy techniques and percutaneous fine-needle
aspiration (FNA) testis “mapping.” As a single testis biopsy is subject to
sampling error, the principle underlying these advanced approaches is to reduce
this error by more intensive sampling. In return, sperm detection rates of 60%
or more are obtained. With the multibiopsy method, four to six individual
testis biopsies are taken from different areas of the testis to increase the
odds of finding sperm in any particular tissue sample.
Similar to other “open” or percutaneous testis biopsy methods, fine-needle
aspiration mapping is performed under local anesthesia. Unlike these
techniques, however, smaller tissue samples are obtained that are then examined
cytologically instead of histologically. It is also a diagnostic procedure that
creates a geographical “map” of the testis to justify future and potentially
more invasive attempts at sperm retrieval. FNA mapping involves wrapping the
testis and scrotal skin
with a gauze wrap posteriorly. The “testicular wrap” is a convenient
handle to manipulate the testis and also fixes the scrotal skin over the testis
for the procedure. Percutaneous aspiration sites are marked on the scrotal
skin, 5 mm apart, according to a template. The number of aspiration sites
varies with testis size and ranges from 4 (to confirm obstruction) to 15 per
testis (for nonobstructive azoospermia). FNA is performed with a
sharp-beveled, small-gauge needle using the established suction cutting
technique. Precise, gentle in-and-out movements are
used to aspirate tissue fragments. After aspiration, the tissue fragments are
expelled onto a slide, gently smeared, and fixed in 95% ethyl alcohol. Pressure
is applied to each site for hemostasis and a routine Papanicolaou stain is
performed and the slides read by a cytologist for the presence or absence of
mature sperm with tails. If sperm are detected, then sperm retrieval can
proceed at the time of IVF-ICSI with a very high possibility of finding sufficient sperm for all oocytes
retrieved.