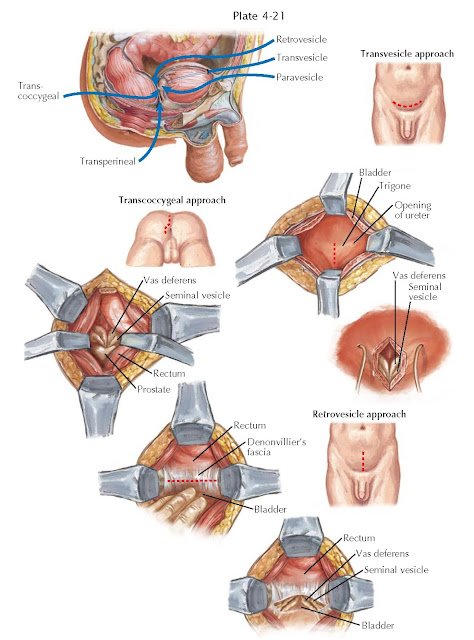
SEMINAL VESICLE SURGICAL APPROACHES
The seminal vesicle is a uniquely male organ, derived from the mesonephric duct (see Plate 1-2) beginning at 13 fetal weeks. The normal adult seminal vesicle is 5 to 8 cm in length and 1.5 cm in width and has a volume of 10 mL. The blood supply is derived from the deferential artery or, occasionally, from branches of the inferior vesical artery. The seminal vesicles receive innervation from adrenergic fibers via the hypogastric nerve.
Primary pathologic states of the organ are rare. Congenital lesions
include ureteral ectopy, cysts, and aplasia, many of which can be observed.
Infections of the seminal vesicles are uncommon, but tuberculosis and
schistosomiasis can cause masses, abscesses, and calcifications. Primary benign
tumors include papillary adenoma, cystadenoma, fibroma, and leiomyoma. Malignant
neoplasms are extremely rare and include papillary adenocarcinoma and sarcoma.
Radical excision of the organ is the standard treatment for malignancy. Far
more common than primary malignancy is secondary involvement from
adenocarcinoma of the bladder, prostate or rectum, and lymphoma. Few
established alternatives to surgery exist for seminal vesicle tumors. A variety
of open surgical approaches to the seminal vesicles have been described,
including transvesical, transperineal, paravesical, retrovesical, and
transcoccygeal methods. In addition, a laparoscopic retrovesical approach is
rapidly gaining in popularity. The chosen approach depends on the nature of the
lesion to be excised and surgeon
experience.
Transvesical approach. With the patient supine, an infraumbilical,
extraperitoneal incision is made, the rectus muscles separated, and the space
of Retzius entered. A Balfour retractor exposes the anterior bladder wall,
which is then opened with a vertical incision. The retractor is repositioned
within the bladder to expose the trigone and posterior bladder wall. With a
cutting Bovie, a vertical incision is made through the trigone near the bladder
neck and the ampullae of the vasa deferentia are visualized posteriorly. The
seminal vesicles are identified lateral to the ampullae, dissected free,
ligated, and divided. A metal clip placed across the cut end of the seminal
vesicle minimizes organ spillage. The distal vascular pedicle is identified and
controlled with clips or ties, and the organ removed. Too deep a dissection
risks violating Denonvilliers fascia and entering the rectum.
Transperineal approach. This approach to seminal vesiculectomy is
virtually identical to that described for radical perineal prostatectomy (see
Plate 4-18). To adequately expose the seminal vesicle, the rectum should be
dissected off the posterior prostate to a point higher than that needed for
perineal prostatectomy. The vasal ampullae can be spared for the excision of a
simple seminal vesicle cyst or small tumor but may need resection in the
setting of cancer or infection.
Paravesical and retrovesical approaches. The paravesical approach
commences with an infraumbilical incision to expose the space of Retzius, and
the bladder is bluntly dissected away from the pelvic side wall. The vas
deferens is tracked medially toward the bladder base to help locate the seminal
vesicle. The plane between the bladder and seminal vesicle is developed from later-
ally to medially. As the seminal vesicle is dissected, the awareness that the
vas deferens crosses over the ureter helps avoid ureteral injury. The bladder
is rolled medially for better exposure. The neck of the seminal vesicle is
defined at the prostate base and the organ ligated with absorbable suture.
The retrovesical approach is appropriate for bilateral seminal vesicle
excision of small cysts or tumors. A midline, infraumbilical, intraperitoneal
incision is made to gain access to the bladder dome and the cul-de-sac between
bladder and rectum. The small and large bowel are packed superiorly, and the
peritoneal reflection near the posterior bladder is incised over the rectum.
With sharp dissection, the bladder is peeled forward off the rectum until the
ampullae and the seminal vesicle apices are visualized. In a manner similar to
the paravesical approach, the seminal vesicles are dissected to the prostatic
base and the organ ligated. The retrovesical approach can also be performed
laparoscopically (see Plate 4-20). Transcoccygeal approach. Less commonly used,
this dissection is appropriate for individuals in whom the perineum or lower abdomen is not accessible because of limitations in
patient positioning or due to multiple prior surgeries. With the patient in the
prone, jackknife position, an incision is made along the coccyx and angled into
a gluteal cleft. The coccyx is removed, and the gluteus maximus muscle
retracted laterally to expose the rectosigmoid colon. After Denonvilliers
fascia is incised deep to the rectum, it is dissected off the prostate with
exposure of the seminal vesicles. Injury to the neurovascular bundle is more
likely with this approach because it is directly in the path of dissection.
After the seminal vesicles are removed, the rectum is carefully inspected for
injury. The wound is closed in anatomic layers, and a drain is placed.