SCOLIOSIS
Scoliosis is a rotational deformity of the spine and ribs. While in most cases the cause of scoliosis is unknown (idiopathic scoliosis), in excess of 50 genetic markers have been identified as having a major role in adolescent idiopathic curves. Scoliosis may also result from a variety of congenital, neuromuscular, mesenchymal, and traumatic conditions, and it is commonly associated with neurofibromatosis.
PATHOLOGY
A complicated three-dimensional deformity, scoliosis is characterized by
both lateral curvature and vertebral rotation. Although degree of vertebral
rotation and lateral curvature do not necessarily proceed in concert,
typically, as the curve progresses, the vertebrae and spinous processes in the
area of the major curve rotate toward the concavity of the curve (see Plates 1-36 and 1-37). Because the
ribs are attached to the vertebral body, the ribs subsequently rotate dorsally
on the convexity and volarly on the concave side. The entire thoracic cage can
become ovoid, and anterior prominence can become as noticeable as posterior
prominence. Most idiopathic curves are noteworthy for relative hypokyphosis of
the thoracic spine. Kyphotic curves are more common in congenital and certain
neuromuscular conditions. Lordosis (swayback) of the lumbar spine may accompany
the scoliotic deformity.
In addition to rotation, scoliosis also causes other pathologic changes
in the vertebrae and related structures in the area of the curve. The disc
spaces become narrower on the concave side of the curve and wider on the convex
side. The vertebrae also may become wedged (i.e., thicker on the convex side).
On the concave side of the curve, the pedicles and laminae are frequently
shorter and thinner and the vertebral canal is narrower.
The structural changes described are most common in idiopathic forms of
scoliosis; the pathologic process may vary somewhat in paralytic and congenital
forms. Generally, in the paralytic curve, which is caused by severe muscle
imbalance, the ribs assume an almost vertical position on the convex side.
IDIOPATHIC SCOLIOSIS
About 85% of patients with scoliosis exhibit an idiopathic (genetic)
form. The disease is not primarily a problem of bone and joints but likely a
manifestation of genetically mediated neuromuscular imbalance. Significant
scoliosis (i.e., curves severe enough to require treatment) occurs up to seven
times more often in girls than boys, whereas mild scoliosis affects boys and
girls in equal numbers.
About 90% of all idiopathic curves are probably genetic, and thus the
two terms are used synonymously. The scoliotic trait may not pass on to every
generation (incomplete penetrance) and may cause a severe curve in a parent and
a mild curve in a child, or vice versa (variable expressivity). If a person
with idiopathic scoliosis has children, about one third of all offspring will
have scoliosis; if both parents have genes for scoliosis, even if one parent
does not exhibit the disease, the odds that offspring will be afflicted are
even greater.
Curve Patterns
For years, the curve pattern classification system used to evaluate
adolescent scoliosis was as described by Moe, Winter,
and King the so-called King classification. In recognition of subtleties with
newer surgical management of advanced curves not well addressed by this older
classification, the Lenke classification system of adolescent idiopathic scoliosis
was developed in an effort to provide a comprehensive and interobserver
reliable means to categorize curves. Upright posteroanterior and lateral
radiographs along with the supine side-bending radiographs are required. The
classification system consists of a triad that utilizes a curve type (1
to 6) (see Plate 1-37), a lumbar spine modifier (A, B, C), and a sagittal
thoracic modifier (−, N, +). All three regions of the radiographic coronal and
sagittal planes the proximal thoracic, main thoracic, and
thoracolumbar/lumbar are designated as either the major curve (largest Cobb
measurement) or minor curves, with the minor curves separated into structural
(rigid correction limited on supine bending films) and nonstructural types
(flexible correction on bending film to < 25 degrees). The
current recommendations are that the
major and structural minor curves be included in the instrumentation and fusion
and the nonstructural minor curves be excluded. Overall, this classification
system is treatment directed; however, there are other aspects of the deformity
that may suggest deviation from the recommendations of the classification
system. The goal of this system is to allow organization of curve patterns to
provide comparisons of treatment methods in order to provide the best treatment
for each scoliosis patient.
 |
| TYPICAL SCOLIOSIS CURVE PATTERNS |
In general, right thoracic curves are the most common. The curve
usually extends to and includes T4, T5, or T6 at its upper end and T11, T12, or
L1 at its lower limit. Typically, these curves do not correct on side bending.
Because of severe vertebral rotation, the ribs on the convex side become badly
deformed, resulting in a severe cosmetic defect and serious impairment of
cardiopulmonary function when the curve exceeds 60 degrees. Right thoracic curves
can develop rapidly and therefore must be treated early.
The right thoracic curve is always a major curve (i.e., the curve
is structural and of great significance). There are usually smaller curves in
the opposite direction above and below the right thoracic curve. These secondary
curves are usually
referred to as minor curves. A minor curve usually forms as a
compensatory mechanism to help keep the head aligned over the pelvis and may be
structural or nonstructural.
The thoracolumbar curve is also a fairly common idiopathic curve
pattern. It is longer than the right thoracic curve and may be to either right
or left. The upper end of the curve extends to and includes T4, T5, or T6 and
the lower end includes L2, L3, or L4, usually with minor upper thoracic and
lower lumbar curves. The thoracolumbar curve is usually less cosmetically
deforming than the thoracic curve; however, it can cause severe rib and flank
distortion due to vertebral rotation.
The double major curve consists of two structural curves of almost
equal prominence. Double major curves can be any of the following combinations:
right thoracic/left lumbar (most common); right thoracic/left thoracolumbar;
left thoracolumbar/right lower lumbar; and right thoracic/left thoracic (double
thoracic).
The lumbar major curve is quite common and usually runs from T11
or T12 to L5. In 65% of cases, the curve is to the left. The thoracic spine
above the curve usually does not develop a structural compensatory curve and
remains flexible. Lumbar major curves are not very deforming but can become
quite rigid, leading to severe arthritic pain in later life and during
pregnancy.
The extent of deformity varies with the underlying curve pattern,
tending to be most severe with the right thoracic and thoracolumbar curves and
less severe with balanced double major curves. Severe right thoracic and
thoracolumbar curves often produce a marked over- hang of the thorax toward the
convexity of the curve and a rib hump, and the torso tilts to the convex side.
In contrast, with a balanced double major curve, the shoulders are level over
the pelvis, and the rib and lumbar prominences are not too severe. The major
deformity with this type of curve is trunk shortening.
Age at Onset
Idiopathic scoliosis is classified into infantile, juvenile, and
adolescent types according to peak periods of onset. Infantile idiopathic
scoliosis, which occurs between birth and 3 years of age, is usually
noticed in the first year of life. Curiously, it is
far more common in England, usually occurs in
boys, and generally results in a left thoracic curve. The majority of these
curves, thought to be a result of molding in the uterus, resolve spontaneously,
even if untreated. Some, however, progress to severely rigid structural curves
unless treated early and aggressively with serial casting as advocated by Mehta
or with bracing.
Juvenile idiopathic scoliosis occurs between the ages of 4 and 10 and is most often detected at or after age 6. Both sexes are affected equally. Most curves in this group are right thoracic curves. Unless early standing and side-bending radiographs are available, it is almost impossible to distinguish cases of late infantile onset from those of early juvenile onset.
Adolescent idiopathic scoliosis is diagnosed when the
curve is noticed between 10 years of age and skeletal maturity. Many curves
first noticed at this age are probably present before age 10 but are not
recognized until the adolescent growth
spurt. Although adolescent scoliosis occurs in both boys and girls equally, 70%
of cases that progress and need treatment occur in girls. The double major and
right thoracic patterns predominate.
Progression
Idiopathic curves may or may not progress during growth. The risk of
progression may be linked to various factors such as sex, age at onset, delayed
maturation, and vertebral anatomy. Usually, the younger the child is when the
structural curve develops, the less favorable the prognosis will be. In
general, structural curves have a strong tendency to progress rapidly during
the adolescent growth spurt, whereas small, nonstructural curves may remain
flexible for long periods, never becoming severe. Nevertheless, the worst
advice a physician can give a patient with scoliosis is “as soon as you finish
growing, your curve will stop.” In a significant number of adults, scoliosis
remains progressive, eventually causing pain and disability.
The curve is most likely to progress 1 to 2 degrees a year during adult
life; if the curve is greater than 60 degrees at maturity, the curve pattern
throws the trunk out of balance or the patient has extremely poor muscle tone.
Generally, a curve that is less than 30 degrees at age 25 is unlikely to
progress.
CONGENITAL SCOLIOSIS
Congenital scoliosis is probably the result of some form of trauma to
the zygote or embryo in the early embryonic period that causes a vertebral or
extravertebral defect. Because many organ systems develop at the same time,
children with congenital scoliosis almost always have some urinary tract or
cardiac anomaly as well. Children with congenital scoliosis should also be
examined for cervical spine anomalies such as Klippel-Feil syndrome (see Plate
1-33) and scapular deformities such as Sprengel deformity.
Congenital curves must be observed carefully. Although most do not
progress significantly, some become severe and irreversible. Posterior
vertebral defects can be open or closed. The open (dysraphic) defect caused by
myelomeningocele can be very severe and is usually associated with partial or
complete neurologic deficit with paraplegia and urinary tract problems.
 |
| CONGENITAL SCOLIOSIS: CLOSED VERTEBRAL TYPES (MACEWEN CLASSIFICATION) |
Closed vertebral defects are classified into four types (see Plate 1-38): (1) partial
unilateral failure of vertebral formation (wedge vertebra); (2) complete
unilateral failure of vertebral formation (hemivertebra); (3) unilateral
failure of segmentation (congenital bar); and (4) bilateral failure of
segmentation (block vertebra). Other congenital combinations, some of which are
extravertebral (e.g., rib fusions), are so mixed and bizarre they defy
classification.
In hemivertebral conditions, as the anomalous vertebrae grow they cause
the spine to lengthen on the convex side, leading to severe curves. Unilateral
bars can also cause severe curvature. The worst possible congenital curve
results from hemivertebrae on one side of the spine and several unilateral bars
on the opposite side.
The best treatment for a progressive congenital curve is a short,
in-situ spinal fusion performed as soon as progression is
noted.
NEUROMUSCULAR SCOLIOSIS
Neuropathic forms of neuromuscular scoliosis are caused by a
variety of disorders. Muscle imbalance due to poliomyelitis, a lower motor
neuron disease, and cerebral palsy, an upper motor neuron disease, may lead to
severe, long C-shaped curves that may extend from the lower cervical
region to the sacrum. Curves caused by syringomyelia also tend to become quite
severe, often necessitating surgery. Because many patients with syringomyelia
live well beyond their teenage years, treatment is definitely indicated when
progression of the curve is noticed. Occasionally, neurosurgical drainage of
the syrinx can help control the curve.
Myopathic forms of neuromuscular scoliosis are caused by
both progressive and static disorders. The progressive disorders are
exemplified by the muscular dystrophies. These disorders cause muscle
imbalance, generally producing long C-shaped curves. Some children with
scoliosis due to muscular dystrophy are so weak that
their spines appear to collapse when they assume the erect posture. Judicious
bracing or surgery may be helpful in some patients, but the prognosis is always
guarded.
Other neuromuscular forms may be caused by mixed disorders, such as
Friedreich ataxia, in which a muscle imbalance causes muscle weakness plus
overpull by the stronger trunk and paraspinal muscles.
MESENCHYMAL AND TRAUMATIC DISORDERS
Congenital mesenchymal disorders leading to scoliosis can occur with
various types of dwarfism and in Marfan syndrome. Because patients with Marfan
syndrome are usually very tall, their curves can become quite severe. In
osteogenesis imperfecta, the extreme brittleness of the bones results in
hundreds of microfractures of the spine, eventually producing a scoliotic
deformity. Scheuermann disease, if not properly treated, may also lead to a
progressive kyphotic deformity in adolescents (see Plate
1-42).
Direct vertebral trauma such as a fracture with wedging or nerve root
irritation can cause scoliosis. In some instances, the scoliosis may be
secondary to irradiation for cancer treatment that, while saving the child’s
life, destroys the growth plates of the vertebral body, resulting in unequal
growth and causing spinal deformity.
Physical Examination. As part of the
thorough physical examination, the development of secondary sexual
characteristics should be noted. Their presence or absence, in addition to a
height comparison with siblings and parents, can be significant in predicting
future growth patterns. The skin is examined for café-au-lait markings
indicative of neurofibromatosis, and the lumbar spine is searched for pigmented
areas or patches of hair that can indicate an underlying congenital condition,
such as spina bifida or diastematomyelia.
Following the general examination, a more specific examination of the
deformity is done, beginning with evaluation of trunk alignment, which is used
to gauge balance or displacement of the torso (see Plate 1-39). A tape measure
dropped as a plumb line from the occiput can show if the head and trunk are
aligned. In patients with a very severe double major curve, however, alignment
may remain perfect.
 |
| CLINICAL EVALUATION OF SCOLIOSIS |
The shoulder girdle should be examined for symmetry, and scapular
prominence should be noted. The neck-shoulder angle may be distorted by
asymmetry of the trapezius muscle caused by cervical or high thoracic curves.
The type of curve is recorded and its flexibility evaluated on side bending
and distraction. Lifting the patient gently by the head distracts the curve,
allowing the degree of rigidity and flexibility of the spine to be assessed.
Deformities of the thoracic cage are carefully recorded. With the
patient bending forward, a scoliometer is used to measure the rib hump (see Plate 1-39). Anterior
rib and breast asymmetry should also be noted.
Pelvic obliquity must be carefully assessed. It can be nonstructural,
occurring as a result of a habit, or structural, resulting from a lower
limb-length discrepancy. Structural pelvic obliquity can also be caused by
contractures of muscle groups either above or below the iliac crests.
A brief but thorough neuromuscular examination including evaluation of
all reflexes, response to stimuli, and motor capabilities is an important part
of the scoliosis workup. In children with congenital conditions, sensory or
motor loss can indicate an internal spinal condition, such as diastematomyelia.
Decreased vibratory sensation in the limbs is a consistent sign in idiopathic
scoliosis, which is due to a brainstem dysfunction; a more extensive neurologic
examination is usually not warranted. The
findings of the neuromuscular examination should be carefully correlated with
the physical examination of the back. Painful scoliosis is uncommon in
children, and its presence suggests the possibility of osteoid osteoma, spinal
cord tumors, spondylolysis or spondylolisthesis, or infection.
Imaging. A single erect anteroposterior radiograph from the
occiput to the iliac crest is sufficient for the initial examination of a new
scoliosis patient. A spot lateral view of the lumbosacral spine is indicated if
spondylolisthesis or spondylolysis (see Plate 1-44) is suspected. The thyroid,
breasts, and gonads should be shielded and radiation exposure kept to a
minimum.
Side-bending radiographs are taken to distinguish structural from
nonstructural curves. Right side bending allows a right thoracic curve to
uncoil, and the radiograph provides evidence of the suppleness of the ligaments
and other soft tissue structures. Left side bending uncoils a left lumbar
curve. Bending radiographs are typically reserved for preoperative evaluation.
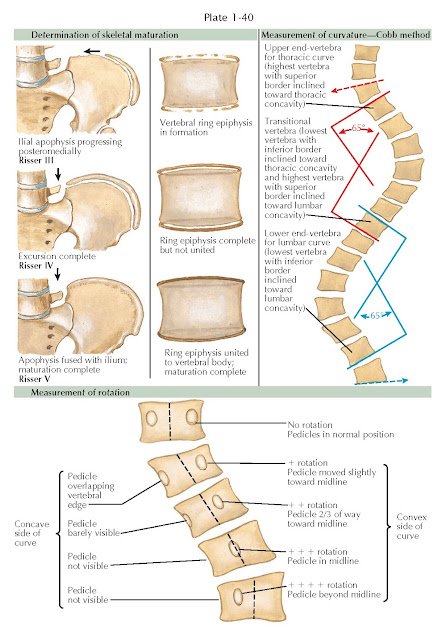 |
| DETERMINATION OF SKELETAL MATURATION, MEASUREMENT OF CURVATURE, AND MEASUREMENT OF ROTATION |
The curve is measured on the initial radiograph using the Cobb method,
which is preferred by the Scoliosis Research Society (see Plate 1-40). The
accuracy of the Cobb method relies on determining the upper and lower
end-vertebrae of the curve. The end-vertebrae at both the upper and lower
limits are those that tilt most severely toward the concavity of the
curve. In other words, the superior end-vertebra is the last vertebra whose
superior border inclines toward the concavity of the curve to be measured and
the inferior end-vertebra is the last one whose inferior border inclines toward
the concavity of the curve. Horizontal lines are drawn at the superior border
of the superior end-vertebra and the inferior border of the inferior
end-vertebra. Perpendicular lines are then drawn from each of the horizontal
lines and the intersecting angles measured. (The broken arrows on Plate 1-40 do not converge
toward the concavity being measured, indicating that these vertebrae are not
end-vertebrae but are in another curve above or below the curve being
measured.)
Vertebral rotation is measured most accurately by estimating
the amount that the pedicles of the vertebrae have rotated, as seen in the
anteroposterior radiograph.
Skeletal maturation must also be determined accurately because scoliosis
progression may slow (although it does not always stop) when a patient is fully
mature. Girls generally cease growing and mature at about 14 12 years of age;
this occurs in boys at age 16 to 17.
Several methods are used to estimate skeletal age. Radiographs of the
left hand and wrist are compared with the Radiographic Atlas of Skeletal
Development of the Hand and Wrist by Greulich and Pyle. Presence of an open
triradiate physis in the acetabulum is an indication of significant skeletal
immaturity. Pelvic radiographs can be used to determine the degree of iliac
crest secondary ossification center excursion known as the Risser sign. When
the iliac crest meets the sacroiliac joint and the physis closes, maturation is
nearly complete. Another technique involves examining the superior and inferior
growth plates of the thoracic and lumbar vertebrae on high-quality radiographs.
If the growth plates are mottled in appearance, the skeletal growth is not
complete. Solid union of the growth plates with the vertebral bodies indicates
that maturation is complete.
Treatment. A variety of treatment modalities are available.
School Screening. The best treatment for scoliosis is early
detection and prompt referral to a center equipped to provide complete
scoliosis care. Most curves can be treated without surgery if detected before
they become too severe. Scoliosis screening is still being done in schools
across the United States and in other countries. A physician, mid-level
provider, or school nurse can typically screen scores of children in less than
an hour. The screening procedure is simple: the child bends from the waist
with the arms hanging freely (see Plate 1-39). This position accentuates even a
slight asymmetry in the ribs or lumbar area. School screening should begin in
the fifth grade, and boys as well as girls should be examined every 6 to 9
months. If scoliosis or kyphosis is detected in a child, all siblings should be
screened.
Exercises. Exercises are mentioned under treatment only to be strongly condemned as a cure for scoliosis. Unfortunately, physicians under the mistaken impression that exercises help to improve or eliminate a curve continue to prescribe an exercise program to many patients, who are then lost to follow-up until their curve becomes more severe. Basically, only two treatments effectively correct scoliosis: spinal bracing and surgery. Braces. With close supervision, a properly constructed, well-fitted brace, such as the Boston, Charleston, or Providence brace, can successfully halt progression of a curve in perhaps 70% of patients, if the patient and family are cooperative. Some curves, however, progress to greater deformity no matter what is done. Unfortunately, there is as yet no way to predict if a curve will respond successfully to bracing.
Low-profile braces have gained broad acceptance among patients and
physicians alike. The now “historical” Milwaukee brace, the first brace
demonstrated to alter the natural history of a curve, is rarely used in the
contemporary management of scoliosis. Patient acceptance is much greater with
these braces because they are barely visible under clothing or worn only at
night. The inner pad is adjustable to add further pressure on the apex of the
curve as the curve improves. The braces can be modified depending on the curve
pattern and the presence or absence of kyphosis.
The Boston brace is generally worn over a long undershirt for 16 hours a
day. Children can run and play in them relatively freely. Exercises are done
daily both in and out of the brace to maintain muscle strength. The Charleston
and Providence brace are “bending braces” that exert corrective force on the
curve by virtue of a side-bending moment.
Patients using braces are seen every 6 months for brace adjustment. At
4- to 6-month intervals, new radiographs are taken with the patient erect and
not wearing the brace. When radiographs show that skeletal maturation is nearly
complete, the bracing is discontinued. Some physicians will stop bracing
abruptly, whereas others wean from the brace. Neither regimen has demonstrated
superiority.
Electrical Stimulation. In years past,
electrical stimulation of muscle gained popularity in the treatment of
scoliosis. It has been abandoned because it was not proven to alter the natural
history of curve progression. In one study, patients who were treated with
electrical stimulation actually fared worse than controls.
Surgery. The main indication for scoliosis surgery is
relentless curve progression—typically progression of thoracic curves in excess
of 45 degrees and progression of thoracolumbar curves to values in excess of 40
degrees. Pain, spinal balance, and general cosmesis are other factors that need
to be considered with respect to surgical decision making. Since the first
spinal fusion was performed in 1911, many different surgical techniques and
types of instrumentation have been developed, each with its own advantages and
risks, including neurologic impairment. Regardless of the method and hardware,
the goal of surgery is to produce a solid arthrodesis of a balanced spine in
the frontal and sagittal planes over a level pelvis.
 |
| BRACES FOR SCOLIOSIS |
Posterior fusion techniques began using Harrington rod instrumentation.
In some patients, a compression rod was added and the rods were further
attached to the vertebrae with wires passed through holes drilled in the
spinous processes. Harrington rods are now primarily of historical interest.
The relative lack of restoration of sagittal balance was a major long-term
problem.
In the Luque technique, still employed in certain neuromuscular curve
types, the spine is straightened with two rods attached to sublaminar wires or
cables. The Cotrel-Dubousset method was the first segmental instrumentation
that allowed for rotation correction of individual spinal elements and employed
two rods coupled together with transverse traction rods and hooks, which
effectively derotated the spine.
Current state of the art instrumentation employs primarily pedicle
screws that in comparison to hooks or sublaminar
wires allow for far greater restoration of sagittal and coronal balance as well
as a more rigid construct that typically obviates the need for postoperative
bracing.
With the broad acceptance of pedicle screw technology as well as the
recognition of its derotational strength, anterior
surgery is less common and is typically reserved for exceptionally rigid curves
requiring disc space release or curves with absent posterior bony elements.
The technique and approach used should be based primarily on
the surgeon’s preference and expertise.





