NONTUBERCULOUS MYCOBACTERIAL LUNG DISEASE
Throughout the 20th century, cases of pulmonary disease caused by mycobacteria other than Mycobacterium tuberculosis were described. Prominent among the “atypical” species have been Mycobacterium avium, Mycobacterium intracellulare, and Mycobacterium kansasii. Unlike M. tuberculosis (which has no common reservoir other than infected humans and is spread exclusively by human-to-human aerosols), the nontuberculous mycobacterial (NTM) lung diseases are found widely distributed in water and soil and appear to be acquired from these environmental sources.
The clinical and radiographic features of NTM disease
are distinctive. Among the traditional male patients, the illness is mindful of
classic TB: upper lobe fibronodular-cavity disease associated with productive
cough, hemoptysis, fever, sweats, and weight loss. By contrast, the prototypic
female case primarily involves bronchiectasis and centrilobular nodules
associated with productive cough and malaise.
EPIDEMIOLOGY
Unlike tuberculosis (TB), for which there are
carefully compiled annual data, there is less reliable information on the
prevalence and distribution of NTM lung disease. A major issue is that not all
patients whose sputum yields an NTM on culture have true “disease,” and, in
fact, 50% to 80% of patients with positive NTM cultures may actually be
“contaminated” by these environmental microbes.
However, many U.S. clinicians believe that they are
seeing more cases, especially among women. In Canada, although the incidence of
pulmonary NTM is roughly 60% that of TB, the prevalence of NTM lung disease
over the next decade is estimated to become substantially greater than that of TB.
This is because of many factors more than 80% of TB cases are treated and cured within
9 months, the observed incidence of TB is decreasing, cure rates for NTM lung
disease are probably in the range of 50% to 60%, and treatment failure or
relapses are common. Hence, an accumulation of NTM patients in Canada and the
United States over time is expected.
Additional emphasis should be placed on the fact that
most TB patients started on therapy rapidly become and remain asymptomatic. By
contrast, many NTM patients with bronchiectasis have protracted symptoms and,
even if the NTM is cured or suppressed, they experience intercurrent
infections, commonly with gram-negative bacilli such as Pseudomonas
aeruginosa.
NONTUBERCULOUS MYCOBACTERIAL SPECIES
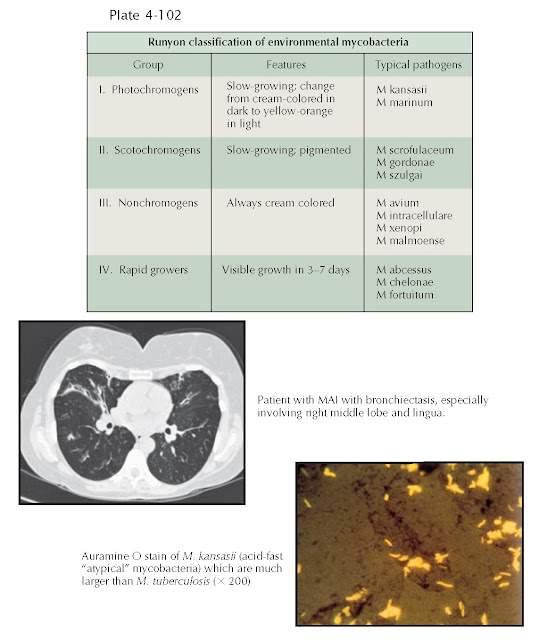
In virtually all recent surveys, the bulk of disease
is associated with M. avium or M. intracellulare. Although
distinct species, these organisms are so similar that they are referred to as M.
avium complex (MAC) or MAI.
M. kansasii has been a
prominent pathogen in the south-central United States but seems relatively less
common in recent experience. Rapidly growing mycobacteria (group IV in the Runyon
system) are being seen with increasing frequency; Mycobacterium abscessus is
much more common than Mycobacterium chelonae. Other NTM that seem to
vary in prevalence regionally include Mycobacterium xenopi, Mycobacterium
simiae, Mycobacterium
malmoense, and Mycobacterium szulgai.
DIAGNOSTIC CRITERIA
Given the potential for contamination, the American
Thoracic Society (ATS) has established criteria for clinical relevance, which
include typical symptoms, suitable radiographic findings (cavities,
bronchiectasis, scattered nodular opacities) and two or more positive sputum
cultures or one positive bronchial aspirate or wash. The clinical significance
is enhanced if it is one of the more common pathogens. Mycobacterium gordonae,
by contrast, is almost universally a contaminant.
Distinctive Morphotype
Two of the most intriguing aspects of the cases among
women are the physical-anatomic features and racial distribution. Unlike TB,
which is more common among persons of color in the United States, the pre-ponderance
of NTM disease is seen among whites and, less frequently, Asians. There is a
notable paucity among African American individuals. The prototypical patient is
variable tall and slender; subtle scoliosis is common, and many patients have
narrowed antero- posterior distance or pectus excavatum. Mitral valve prolapse
is found with higher than normal frequency.
Although the disease can involve any region of the
lungs, bronchiectasis and volume loss of the right-middle lobe or lingula are
strikingly prominent.
TREATMENT
Antimicrobial therapy is delineated in the 2007 ATS
guidelines. For the slowly growing species (M. kansasii, MAC, M.
xenopi, and so on), regimens composed of clarithromycin (or azithromycin),
RIF, and EMB are usually used. An injectable agent such as amikacin may be
added initially for more extensive disease.
However, for the more common rapidly growing
mycobacterial species such as M. abscessus and M. chelonae, an
intravenous regimen such as imipenem or cefoxitin and either amikacin or
tobramycin appears more efficacious.
For infections caused by the slowly growing mycobacterial
species, therapy usually entails 12 to 18 months of continuous therapy with the
objective of cure. However, the rapidly growing mycobacteria are prone to
recur, and the strategy includes several months of intensive suppressive treatment with the
anticipation of retreatment.