FUNCTIONAL CHANGES IN GASTRIC
MOTILITY AND SECRETION IN GASTRIC
DISEASES
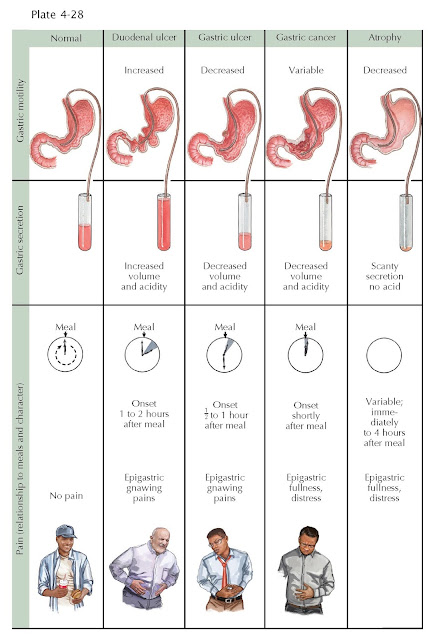
Gastric secretion and motility vary considerably from one individual to another and in the same individual from time to time. In the stomachs of subjects in whom no disease of the upper gastrointestinal tract can be demonstrated, the emptying time of a standard meal may vary over 100% from the average, and the concentration of HCl (acid) secreted in the basal state or in response to the standard stimuli ranges from 0 to 100 mEq/L or more.
A
tendency to gastric hypertonicity and hypermotility is observed in many
duodenal ulcer patients. Initial emptying of a meal may be delayed for a
considerable time because of reflex antral spasm incited from the ulcerated
duodenal bulb; after the pressure by the active contractions of the stomach
overcomes the pyloroantral resistance, evacuation proceeds rapidly, so that the
final emptying time may be considerably shortened. The most important motility
change occurs when the ulcer area becomes inflamed and edematous, or scarred,
so that the gastric outlet is obstructed. After a preliminary period of
hypermotility, the stomach becomes atonic, a condition immediately recognized
roentgenographically with the first swallow of barium. The stomach, in cases of
duodenal ulcer, tends to secrete excessive acid, in both volume and
concentration, so that the average output of acid in duodenal ulcer
patients greatly exceeds the average of all other categories, including the
normal. The rare disease described by Ellison and Zollinger is characterized by
peptic ulceration in the upper intestine distal to the duodenal bulb and
secretion of enormous quantities of gastric acid.
It
is not certain whether hypersecretion exists before the duodenal ulcer starts
to develop, but it does persist after the ulcer heals. This may be due to an
underlying H. pylori infection affecting the inhibitory D cells of the
stomach secreting somatostatin that normally inhibits gastric acid secretion.
The
pain in duodenal ulcer is most often described as a gnawing or intense hunger
sensation, coming on characteristically from 1 to 2 hours after a meal.
The
pathophysiologic phenomena caused by a gastric ulcer depend on the site of the
ulcer in the stomach. The closer the ulcer is to the pylorus, the more the
manifestations resemble those of duodenal ulcer. In peptic ulcer of the lesser
curvature at or proximal to the incisure, gastric motility is not notably
altered from normal, except for some local
hypertonicity of the musculature at, and frequently opposite, the ulcer site.
When the gastric emptying is delayed in a case of ulcer of the body of the
stomach, the presence of a coexisting duodenal ulcer should be suspected. The
gastric stasis resulting from chronic pyloric narrowing by a duodenal ulcer may
be a factor for formation of a gastric ulcer.
The pain of gastric ulcer tends to occur
relatively soon after eating, because the gastric acid content is in immediate
contact with the lesion. For this reason, smoothness and blandness of the diet
are much more important in a gastric than in a duodenal ulcer. Now that proton
pump inhibitors are used in treatment, eating a bland diet has become less
important.
GASTRIC
CANCER
Gastric
carcinoma is not characterized by any general motility pattern, except for the
obvious changes to be expected in an area of infiltration into muscle or where
the tumor produces obstruction.
GASTRIC
ATROPHY
In
atrophy of the gastric mucosa (schematically indicated in the picture by
a flattened mucosal surface, although the thinning of the mucosa by loss of the
normal glandular arrangement does not necessarily result in obliteration of the
rugal folds), the reduction in glandular elements results in greatly
diminished acid secretion and often no HCl secretion even with maximal stimulation.
The reduction of gastric acid results in a secondary elevation of the systemic
hormone gastrin, trying to signal to increase gastric acid secretion. Thus, an
elevated serum gastrin level may be seen in either Zollinger-Ellison syndrome
or pernicious anemia with its gastric atrophy. Differentiation of these two
entails the presence of ulcers in Zollinger-Ellison syndrome or measuring
gastric acidity (low in pernicious anemia but high in Zollinger-Ellison
syndrome). If motility is affected at all in gastric atrophy, it is in the
direction of a decrease.