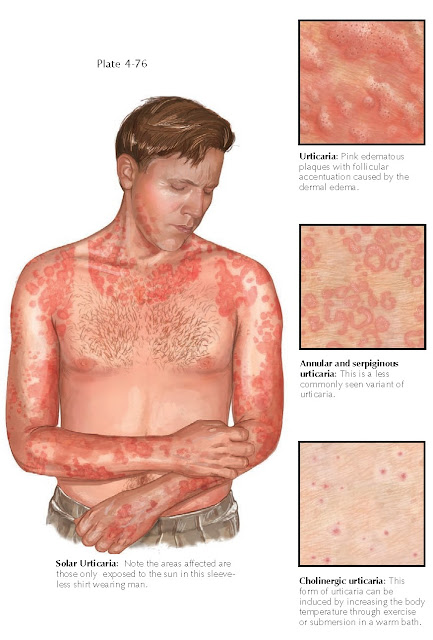
URTICARIA
Urticaria is a commonly encountered skin condition with a multitude of causes. There are primary and secondary forms of urticaria. Most secondary causes are acute in nature and can be explained by an underlying disease state, medication, or food. Urticaria can be a manifestation of many disease states, such as Muckle-Wells syndrome. Urticaria can also be a secondary sequela of an underlying malignancy, acute or chronic infection, genetic disease, and rheumatologic disease. It can also be seen as an acute reaction in a patient with anaphylaxis.
Primary
urticaria can be divided into subsets of disease. The most common type is
chronic idiopathic urticaria. Other forms of primary urticaria include the
physical urticarias. There are many forms of physical urticaria, and the astute
clinician can perform provocative testing to determine the type. There is no
known cure for urticaria, but most cases of primary urticaria spontaneously
resolve within 2 to 3 years.
Clinical
Findings: Primary idiopathic urticaria is one of the most frequently encountered
forms of urticaria. If no underlying cause is found and the urticaria lasts
longer than 6 weeks, it is given the designation chronic idiopathic
urticaria. This form of urticaria comes and goes at will with no
provocative or remitting factors. Lesions appear as evanescent, pink to red,
edematous plaques or hives. They can occur anywhere on the body and can cause
much distress to the patient because of their appearance and because of the
severe pruritus. Patients are particularly distressed when the hives affect the
face and eyelids, causing periorbital and periocular swelling. Patients with
chronic urticaria usually undergo a battery of laboratory and allergy tests. A
complete blood count, metabolic panel, chest radiograph, and measurements of
thyroid-stimulating hormone and antithyroid should be performed, as well as
testing for various infectious diseases if the medical history war- rants.
Testing for hepatitis B, hepatitis C, and HIV infection can be done in the
appropriate clinical setting. Patients with a travel history often undergo
stool examinations for ova and parasites. A full physical examination is
warranted, together with age-appropriate cancer screening. Most patients with
chronic urticaria have no appreciable cause for their hives and are diagnosed
as having chronic idiopathic urticaria.
The physical
urticarias are a group of conditions that cause hives; they represent a unique
form of chronic idiopathic urticaria in that there is a precipitating factor.
There are many types of physical urticaria, including aquagenic and cholinergic
forms and cold-, pressure-, solar-, and vibratory-induced urticaria. These
forms are diagnosed based on the results of provocative testing. The clinical
history often leads to the diagnosis and the appropriate testing regimen. As an
example, a patient may develop hives only under tight-fitting socks. This is
typical for pressure-induced urticaria. If the patient develops hives on
appropriate provocative testing, the diagnosis is made.
Pathogenesis:
The
pathogenesis of urticaria is poorly understood. Mast cells play a critical
role. A stimulus causes mast cells to release histamine, which acts on the
local vasculature to increase vascular permeability. The increased permeability
causes localized swelling. Some forms of urticaria, such as those seen in
anaphylaxis, are caused by a type I hypersensitivity reaction. Other forms of
secondary urticaria may be caused by specific immunoglobulin E (IgE) antibodies
that interact with mast
cells.
Many
medications have been shown to cause mast cell degranulation without an
IgE-mediated pathway. The most common of these are the opiates and anesthetic
agents. Chemical transmitters other than histamine also play a role in
urticaria; they include the leukotrienes, serotonin, and various kinins.
Histology:
The
histological findings in urticaria are bland. The specimen typically shows a
superficial perivascular lymphocytic infiltrate with some dermal edema. The epidermis is
normal.
Treatment:
Treatment
of chronic idiopathic urticaria is based on symptom relief. Antihistamines are
the first-line therapy and can be used in combination. The lack of response can
be frustrating for both patient and physician. Physical urticarias are treated
in the same manner, with emphasis on avoidance. Patients who can avoid exposure
to the physical stimulus responsible for the urticaria have been shown to
have a better clinical outcome.