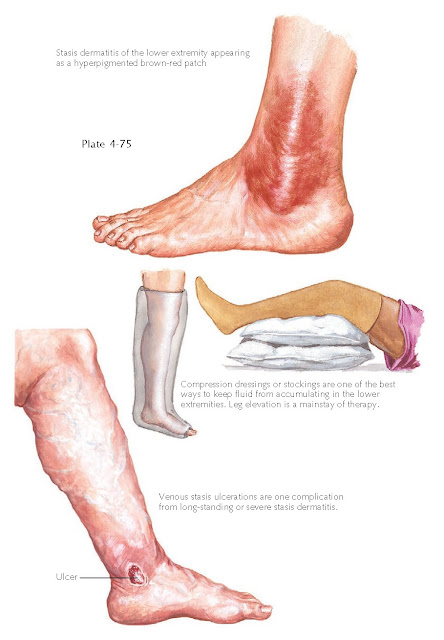
STASIS DERMATITIS
Stasis dermatitis is a common chronic dermatosis that is seen almost exclusively on the lower extremities. The inflammation can lead to chronic discoloration, ulceration, and infection. Underlying systemic disease such as congestive heart failure and renal failure can predispose to stasis dermatitis. Any condition that can cause edema of the lower extremities has the potential to cause stasis dermatitis.
Clinical
Findings: Stasis dermatitis is a chronic inflammatory skin disease that indicates
underlying insufficiency of the venous return system. It is most commonly seen
in the older population, and there is no gender or racial predilection. Most
often, congestive heart failure is the associated disease causing the edema.
Many other conditions of venous insufficiency can also be causative, including
varicose veins and postsurgical complications, such as after a saphenous vein
harvest for coronary artery bypass surgery or an inguinal lymph node
dissection.
Stasis
dermatitis is a skin manifestation of a wide range of underlying venous
diseases. The lower extremities account for more than 99% of cases of stasis
dermatitis, and the diagnosis in other areas of the body should be questioned.
The legs tend to have a range of edema, from the very mild amount that
accumulates at the end of a long day of standing to severe chronic edema that
is always present. Red-brown patches, some with a light yellow discoloration, typically
begin around the medial malleolus. As the condition progresses, the patches
begin to spread and can encompass the entire lower extremity, although much
more commonly they are found at knee level or just below knee level. There can
be complete confluence of the dermatitis around the affected limb, or it can
affect only part of the leg.
The rash is
almost always symmetric, and it is not uncommonly misdiagnosed as bilateral
lower extremity cellulitis. The rash is typically pruritic, and the itching can
be so severe as to cause excoriations and small ulcerations. Depending on the
severity, weeping vesicular patches and plaques can form. A rare bulla can also
be seen in some cases, and one must consider bullous pemphigoid in the
differential diagnosis. Varicose veins are often present on examination, or
there may be a history of bypass surgery. If left untreated, venous stasis can
lead to venous ulcerations, which have been described as slightly painful
ulcerations on the lateral malleolus. The ulcerations can occur anywhere on the
leg and in some cases are very tender. Peripheral pulses are intact, and this
physical examination finding helps to rule out arterial insufficiency. If the
ulcerations and edema are not controlled, the ulcerations will continue to
expand and can become secondarily infected; if they become deep enough, they
can lead to underlying osteomyelitis or cellulitis. These neglected cases can
end in loss of the affected portion of the limb if medical therapies do not
successfully clear the infection and ulcerations.
Pathogenesis:
Increased
pressure within the venous system of the lower extremity causes extravasation
of serum and blood into the surrounding dermis and sub- cutaneous tissue. As
the edema in the lower extremity worsens, the skin begins to develop signs of
chronic inflammation mediated by the abnormal location of fluid.
Histology:
Biopsies
are not routinely performed in stasis dermatitis, and the diagnosis is almost
always made clinically.
Histological examination shows an increase in small vessels, extravasation of
red blood cells, and hemosiderin deposition in the dermis. The epidermis shows
varying amounts of spongiotic dermatitis.
Treatment:
The
rash can be treated symptomatically with topical corticosteroids and
emollients. The main goal of therapy is to restore the proper venous flow.
Depending on
the underlying reason for the stasis dermatitis, this may or may not be
possible. If it is not possible, the mainstay of therapy is the use of
compression stockings or wraps. However, the compliance rate is low because of
difficulty putting them on and discomfort. Those patients who are able to use
the compression gear and topical corticosteroids usually have a good prognosis.