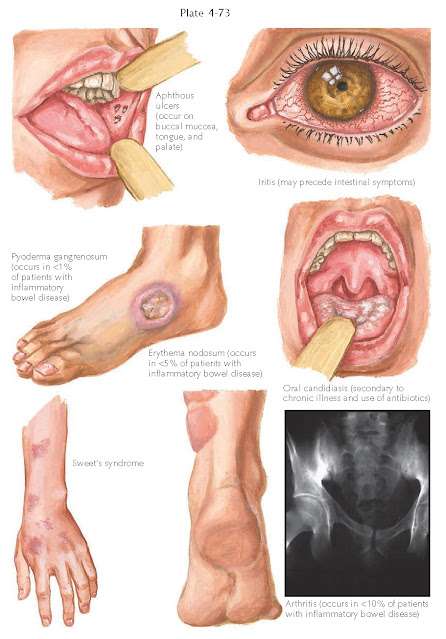
SKIN MANIFESTATIONS OF INFLAMMATORY BOWEL DISEASE
Crohn’s disease and ulcerative colitis are two common autoimmune gastrointestinal disorders with many cutaneous findings. Most patients do not have the cutaneous findings, but a small proportion of the population with inflammatory bowel disease develop one of the cutaneous manifestations, which include pyoderma gangrenosum, aphthous ulcerations, oral candidiasis, erythema nodosum, metastatic Crohn’s disease, iritis, and conjunctivitis. Arthritis, although not a skin manifestation, can produce red, tender swelling around an afflicted joint space.
 |
| MUCOCUTANEOUS MANIFESTATIONS OF INFLAMMATORY BOWEL DISEASE |
Clinical
Findings: Ulcerative colitis and Crohn’s disease are more commonly seen in the
Caucasian population. Crohn’s disease is slightly more common in women, and
ulcerative colitis affects men and women equally. Up to 20% of individuals with
inflammatory bowel disease have a family history of the condition. Ulcerative
colitis affects the large intestine, whereas Crohn’s disease has been shown to
affect any part of the gastrointestinal tract.
Skin
manifestations occur in 5% to 10% of those affected by inflammatory bowel
disease. The most common skin finding is erythema nodosum. Erythema nodosum
manifests as tender dermal nodules predominantly on the shin region. They
typically are symmetric in location. There are many associations with erythema
nodosum in addition to inflammatory bowel disease, including pregnancy, use of
birth control medications, sarcoidosis, deep fungal infections such as coccidiomycosis,
and an idiopathic form. The etiology and pathogenesis are unknown. Erythema
nodosum can occur in areas other than the pretibial region, but this is
uncommon.
Pyoderma
gangrenosum is one of the most severe skin manifestations of inflammatory bowel
disease. It can manifest as a small, red papule or pustule that can rapidly
expand to form a large ulceration with a violaceous undermined rim. The ulcer
may form in a cribriform pattern. The skin involved develops small cribriform
ulcerations centrally that expand outward and coalesce into one large ulcer.
These ulcers are extremely tender and cause significant morbidity. Pyoderma
gangrenosum can also be seen as an idiopathic finding or in association with an
underlying malignancy, typically in the lymphoproliferative group of
malignancies. It has been estimated that approximately 1% of patients with
inflammatory bowel disease will develop pyoderma gangrenosum.
Aphthous
ulcers can occur anywhere within the oral mucosa. They are shallow ulcerations
with a white fibrinous base. They are quite tender and can cause patients to
avoid eating because of the severe discomfort. Oral candidiasis is typically an
iatrogenic manifestation of inflammatory bowel disease. Most patients are
prescribed systemic steroids to treat their underlying disease, and this
predisposes them to the development of Candida infections, both oral and
vaginal.
Arthritis is
seen in approximately 10% of patients with inflammatory bowel disease and is
considered to be in the seronegative classification of inflammatory
arthropathies.
Metastatic
Crohn’s disease is unique to Crohn’s. It represents the spread of the
granulomatous disease onto the skin. It most commonly occurs in areas with
close approximation to the gastrointestinal tract, such as the perianal and
perioral regions. It manifests as tender, draining papules and nodules. A peculiar variant has been described to
occur along the inguinal creases. It appears as fissures or ulcerations that
can penetrate deeply into the dermis and even the subcutaneous fat tissue. It
has been described as slit-like or knife-like linear ulcerations. Isolated
genital swelling is another unusual presentation of metastatic Crohn’s disease.
Metastatic Crohn’s disease has been described in many other cutaneous
locations. This form of cutaneous disease can be difficult to treat.
Other rare
skin findings that have been seen in association with inflammatory bowel
disease are skin fistulas, vasculitis including polyarteritis nodosa,
urticaria, Sweet’s syndrome, epidermolysis bullosa acquisita, and psoriasis.
 |
| CUTANEOUS MANIFESTATIONS OF INFLAMMATORY BOWEL DISEASE |
Pathogenesis:
The
pathogenesis of these cutaneous manifestations of inflammatory bowel disease is
unknown. They are theorized to be caused by an autoimmune mechanism of
defective cell-mediated immunity. Metastatic Crohn’s disease is believed to be
caused when the inflammatory
bowel disease recognizes the skin as gut tissue and develops the same
granulomatous process within the cutaneous structures.
Histology:
Pyoderma
gangrenosum shows non-specific ulceration when biopsied. The findings are nondiagnostic, and the
diagnosis is one of exclusion. The presence of multiple neutrophils leads one
to look for cutaneous infection, and appropriate tissue cultures should be
performed and found negative before a diagnosis of pyoderma gangrenosum is
made. The appearance of pyoderma gangrenosum histologically is highly dependent
on the time and type of lesion biopsied. Early lesions show a follicle-centered
neutrophilic infiltrate with a dermal abscess. As the lesions progress,
ulceration is seen with a predominant neutrophilic infiltrate. The ulcers are
often very deep and enter the subcutaneous tissue. Changes of vasculitis can
often be seen, but they are believed to be caused by the overlying ulceration;
the vasculitis is not thought to be the predominant pathological process.
Biopsy
specimens of erythema nodosum shows a septal panniculitis. The fibrous septa are inflamed with a mixed
inflammatory infiltrate with heavy lymphocyte predominance. Giant cells are
frequently seen within the widened septal tissue. A unique finding is that of
Miescher’s radial granuloma formation, in which multiple histiocytes are
arranged flanking a small area. They are organized circumferentially around a
central slit-like space. The reason for this finding is unknown. Erythema
nodosum is the most common form of septal panniculitis.
Aphthous
ulcerations, if biopsied, show small ulcerations or erosions of the mucosa. The
predominant cell type found within the infiltrate is the neutrophil. These findings
are nonspecific.
Oral
candidiasis should be diagnosed without a skin biopsy. A scraping of the white
oral plaques shows an easily removed, whitish, sticky tissue. A microscopic
examination shows candidal elements. Examination of the biopsy specimen shows
the candidal organisms on the surface of the mucosa, with an underlying mixed
inflammatory infiltrate.
Metastatic
Crohn’s disease is a unique phenomenon. It is histologically described as
noncaseating granulomas. These granulomas are identical to the bowel
granulomas. The skin granulomas are centered in the dermis but can be seen
around blood vessels and into the adipose tissue.
Treatment:
Therapy
is aimed at controlling the underlying bowel disease. If it is well controlled,
the skin manifestations typically follow in line. Conversely, if the bowel
disease is poorly controlled, one can expect the skin disease to be poorly
controlled as well. It is useful to use the skin manifestations as a sign of
active bowel disease. If a patient who has been in a long remission suddenly
develops pyoderma gangrenosum, it is highly plausible that the bowel disease
has become active once more. Ulcerative colitis can be cured by colectomy.
Crohn’s disease cannot be cured by colectomy because it affects the entire
gastrointestinal tract. Oral or intravenous immunosuppressive medications are
used to treat both these conditions. Oral prednisone, sulfasalazine,
azathioprine, methotrexate, myco- phenolate mofetil, and intravenous infliximab
have shown excellent results in patients with these chronic diseases. They also
have the added benefit of helping the skin disease. Cyclosporine and prednisone have shown excellent
results in treating pyoderma gangrenosum. Intralesional triamcinolone can be
attempted on small, early lesions of pyoderma gangrenosum.
Oral
aphthous ulcers can be treated with topically applied steroid gels or ointments
compounded in dental paste formula to increase adherence to the mucosa. Topical
anesthetics are commonly used.
Erythema
nodosum can be treated with compression stockings, topical potent steroids, and
oral steroids in severe cases. Intralesional injection of triamcinolone is also
effective. Metastatic Crohn’s disease is difficult to treat and requires
systemic immunosuppressive agents such as azathioprine, prednisone, or
infliximab. It is best treated by a multi-disciplinary approach.




