HYPERTENSION
Hypertension is a disorder of BP regulation that results from an increase in cardiac output, or most often, an increase in total peripheral vascular resistance. Cardiac output is usually normal in established essential hypertension, although increased cardiac output plays an etiologic role. The phenomenon of autoregulation explains that an increase in cardiac output causes persistently elevated peripheral vascular resistance, with a resulting return of cardiac output to normal. Fig. 15.1 shows mechanisms that can cause hypertension. Inappropriate activation of the renin-angiotensin system, decreased renal sodium excretion, and increased sympathetic nervous system activity, individually or in combination, are probably involved in the pathogenesis of all types of hypertension. Hypertension also has genetic and environmental causes; the latter includes excess sodium intake, obesity, and stress. The inability of the kidney to optimally excrete sodium, and thus regulate plasma volume, leads to a persistent increase in BP whatever the etiology.
Many older adults with elevated BP have isolated systolic hypertension,
which is a systolic pressure that is ≥130 mm Hg with a normal diastolic
pressure. Stiffening of large arteries and increased systolic pulse wave velocity elevate systolic BP,
increase myocardial work, and decrease coronary perfusion.
FIG
15.1 Factors Involved in the Control of
Blood Pressure. CO, Cardiac output; PR, peripheral resistance.
CLINICAL PRESENTATION
Most patients with early hypertension have no symptoms attributable to
high BP. However, long-term BP elevation often leads to hypertensive heart
disease, atherosclerosis of the aorta and peripheral vessels, cerebrovascular
disease, and chronic kidney disease.
Left ventricular hypertrophy (LVH) is the principal cardiac manifestation
of hypertension. Increased left ventricular (LV) mass can be identified by
echocardiography in nearly 30% of unselected hypertensive adults and in most
patients with long-standing, severe hypertension. LVH is more prevalent in men
and more common in black individuals than in white individuals with similar BP
values. Increasing age, obesity, high dietary sodium intake, and diabetes are
also associated with cardiac hypertrophy.
Increased ventricular afterload resulting from elevated peripheral
vascular resistance and arterial stiffness is considered the principal
determinant of myocardial hypertrophy in patients with hypertension.
Hemodynamic overload stimulates increases in myocyte size and the synthesis of
contractile elements. Fibroblast proliferation and deposition of extracellular
collagen accompany these cellular changes and contribute to ventricular
stiffness and myocardial ischemia. A growing body of evidence suggests that
angiotensin II and aldosterone, independent of pressure overload, stimulate
this interstitial fibrosis (Fig. 15.2).
 |
FIG 15.2 Myocardial
Fibrosis. ACE, Angiotensin-converting enzyme; ACE-I, angiotensin-converting enzyme inhibitor; ANG I, angiotensin I; ANG II, angiotensin II.
Clinical consequences of hypertensive heart disease include heart failure and coronary heart disease (CHD). More than 90% of patients with heart failure have hypertension, and data from the Framingham Heart Study suggest that high BP accounts for almost one-half of the population burden of this disorder. Treating hypertension reduces the risk of heart failure by nearly 50%. Heart failure develops because of the myocyte hypertrophy and ventricular fibrosis that characterize hypertensive LVH. As illustrated in Fig. 15.3, the early functional manifestations of LVH include impaired LV relaxation and decreased LV compliance. Although the ejection fraction is preserved initially, diastolic dysfunction often results in increased filling pressures, leading to pulmonary congestion. This mechanism accounts for the symptoms observed in approximately 40% of hypertensive patients with heart failure. If excessive BP levels persist, myocyte loss and fibrosis contribute to ventricular remodeling and contractile dysfunction. Compensatory mechanisms, including remodeling of the peripheral vasculature and activation of the sympathetic nervous and renin-angiotensin systems, accelerate the deterioration in myocardial contractility. Ultimately, decompensated cardiomyopathy and heart failure from systolic dysfunction develop.
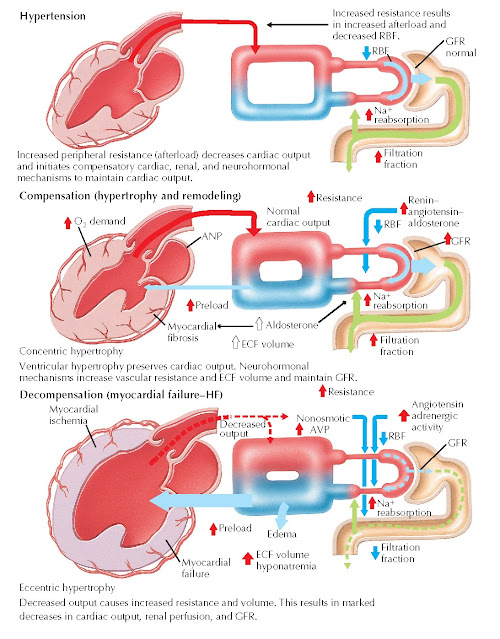 |
FIG 15.3 Hypertension
and Heart Failure (HF). ANP, Atrial natriuretic peptide; AVP, arginine vasopressin; ECF, extracellular fluid; GFR, glomerular filtration rate; Na, sodium; RBF, renal blood flow.
CHD is approximately twice as prevalent in hypertensive individuals as in normotensive individuals of the same age. CHD risk increases in a continuous and graded fashion with both systolic BP and diastolic BP. A reduction in diastolic BP of 5 mm Hg with drug therapy decreases the incidence of myocardial infarction (MI) by approximately 20%. Multiple factors contribute to the enhanced risk of CHD associated with high BP: atherosclerotic narrowing of epicardial coronary arteries is accelerated; coronary arteriolar hypertrophy, reduced myocardial vascularity (rarefaction), and perivascular fibrosis limit coronary arterial flow reserve and predispose the LV to ischemia; and impaired coronary endothelial function increases coronary tone. MI and chronic ischemia contribute to LV dysfunction, increasing the risk of heart failure and cardiovascular death.
Approximately 95% of patients with elevated arterial pressure have
hypertension of unknown etiology, which is known as essential hypertension. The
remaining 5% have an identifiable cause of secondary hypertension (Box 15.2). Although relatively few patients have
secondary hypertension, identification of these patients is important, because
their hypertension
can often be cured or significantly ameliorated by an interventional procedure,
a specific drug therapy, or stopping a culprit drug. Identifiable causes of
hypertension should be sought in the initial history, physical examination, and
laboratory studies. Further diagnostic evaluation for secondary hypertension
causes is pursued when the presentation is atypical for essential hypertension
or when the initial evaluation suggests an
identifiable cause (Box 15.3).
DIAGNOSTIC APPROACH
Objectives of the initial evaluation of a hypertensive patient include
confirmation of hypertension, evaluation of the presence and extent of target
organ disease, identification of cardiovascular risk factors and coexisting
conditions that influence prognosis and therapy, as well as exclusion or
detection of identifiable causes of elevated BP. These goals can usually be
achieved with a comprehensive history, a thorough physical examination, and selected laboratory
studies (Box 15.4).
Detection and diagnosis of hypertension begin with accurate office measurements of BP. Measurements should be
acquired at each encounter, with follow-up determinations at intervals based on
the initial level. Accurate equipment and proper technique, as described in Box
15.5, are critical. Measurement in the upper arm with an oscillometric device
is preferred over auscultatory methods, and automated office BP measurement
(AOBP) the use of an automated device
that measures BP repeatedly in the absence of a healthcare professional is optimal. Before treatment with
medication is initiated, high BP should be confirmed with measurements outside
the office setting. Ambulatory BP monitoring (ABPM) (Box 15.6), a technique by
which BP is measured over the course of a typical day using a small, portable
machine worn by the patient, is the best method for diagnosing hypertension.
Confirmation of high BP with home BP monitoring (HBPM) (Box 15.7), with
measurements acquired systematically using a validated, automated device, is
also acceptable. Both ABPM and HBPM are more reproducible, correlate more
closely with target organ damage, and are more predictive of cardiovascular
events than measurement of BP in the office. Approximately 20% of patients
believed to have hypertension on the basis of office measurements have lower BP
outside the office setting and do not require medical therapy. Conversely, some
patients have “masked” hypertension, with high BP for most of the day despite
normal office levels.
MANAGEMENT AND THERAPY
The principal goal of hypertension treatment is to reduce the risk of
cardiovascular morbidity and death. The treatment approach is determined not
only by the level of BP, but also the presence of other major cardiovascular
risk factors and target organ damage. Lower risk patients with mild BP
elevations may benefit from a period of observation and lifestyle modification,
using medical therapy if the average BP exceeds 140/90 mm Hg over months of
monitoring. The 2017 Hypertension Guideline recommends a medication treatment
threshold of 130/80 mm Hg in patients with a high absolute risk of
cardiovascular events that is, those with clinical
cardiovascular disease (coronary heart
disease, heart failure, or stroke), diabetes, chronic kidney disease (stage 3
or higher or stage 1 or 2 with albuminuria [≥300 mg/d, or ≥300 mg/g albumin-to-creatinine ratio]),
or a calculated 10-year atherosclerotic vascular disease risk exceeding 10%. A
treatment threshold of 140/90 mm Hg is reasonable in individuals with confirmed
hypertension but lower cardiovascular risk. A target BP <130/80 mm Hg is
recommended in most patients. However, in selected patients at high risk, a
goal systolic BP of <120 mm Hg may be appropriate.
Lifestyle modifications are an important component of therapy for high
BP. All patients with hypertension, high-normal BP, or a strong family history
of hypertension should be encouraged to adopt the measures outlined in Box 15.8.
These lifestyle changes are proven to lower
BP and may reduce the need for drug therapy, enhance the effectiveness of antihypertensive drugs, and favorably
influence other cardiovascular risk factors. Other measures, including smoking
cessation and reduced intake of saturated fats, may further reduce
cardiovascular risk.
Pharmacological treatment of hypertension reduces the incidence of heart
failure, stroke, and MI, and decreases the mortality rate due to cardiovascular
causes in middle-aged and older adults. Drug therapy is indicated if lifestyle
modifications do not bring BP into the desired range within a reasonable period
of time. Thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors,
angiotensin-receptor blockers (ARBs), and calcium antagonists are appropriate
first-line agents. Thiazide diuretics and calcium antagonists are preferred in
black patients who do not have a specific indication for an ACE inhibitor or
ARB. In many patients, the choice of
a drug is influenced by comorbid conditions. Table 15.1 lists
agents that are preferred or relatively contraindicated in specific
circumstances.
Many patients with hypertension have established cardiovascular disease,
and their treatment regimen should include medications that control symptoms,
slow disease progression, and prevent cardiovascular events. Treatment
strategies for patients with ischemic heart disease or heart failure are addressed in Chapters 19 and 29.
β-blockers and ACE inhibitors mitigate symptoms and prolong survival in
patients with CHD or LV dysfunction. ARBs are an effective alternative in
patients with heart failure who cannot tolerate ACE inhibitors. Aldosterone
antagonists are beneficial in patients with LV dysfunction or a history of MI.
Calcium antagonists are useful adjuncts in patients with angina or hypertension
that cannot be con- trolled by β-blockers and ACE inhibitors. The optimal
therapy for patients with heart failure with preserved ejection fraction is not
well established and is under investigation; agents that treat LV systolic dysfunction,
especially aldosterone antagonists, seem to be useful. Lowering BP with any of
the first-line drugs leads to LVH regression.
The optimal target BP in patients with isolated systolic hypertension and
chronic ischemic heart disease is controversial. In general, lower values of
systolic BP are associated with better outcomes. However, myocardial perfusion
occurs almost exclusively in diastole, and excessive lowering of diastolic BP
in patients with obstructive coronary disease could theoretically result in
ischemia and increase the risk of coronary events. Several studies have
suggested a J-shaped relationship between diastolic BP and coronary risk, with
an increase in events as diastolic BP is lowered to <80 mm Hg. These
observations have led some experts to caution against aggressive BP lowering in
patients with isolated systolic hypertension and ischemic heart disease.
 |
FIG 15.4 Combinations
of Classes of Antihypertensive Drugs. Green continuous line, preferred combination; green dashed line, useful combination (with some
limitations); black dashed lines,
possible but less well-tested combinations; red continuous line, not recommended combination. ACE, Angiotensin converting enzyme.
In general, therapy with antihypertensive drugs should be initiated at low doses to minimize side effects. Long-acting formulations with 24-hour efficacy are preferred over shorter acting agents because of greater patient adherence to once-daily dosing regimens and more consistent BP control throughout the day. Based on patient response, the dose of the initial agent can be slowly titrated upward, or a small dose of a second agent can be added. Most patients with hypertension require multiple drugs for optimal BP control. Effective drug combinations use medications from different classes and result in additive BP-lowering effects, while minimizing dose-dependent adverse effects. Thiazide diuretics potentiate the effect of ACE inhibitors, ARBs, and calcium antagonists; other useful combinations include calcium antagonists and ACE inhibitors or ARBs. A combination of an ACE inhibitor or ARB plus a thiazide diuretic and calcium antagonist is often effective in patients who require three drugs. Recommended combinations of antihypertensive medications are illustrated in Fig. 15.4.
Resistant hypertension is defined as a properly measured BP that remains
above goal despite the adherence of patients to a regimen of three optimally
dosed antihypertensive agents of different classes, one of which is a diuretic.
The true prevalence of resistant hypertension is not known, but it is probably
present in approximately 15% of treated patients with hypertension. These
patients are more likely to have target organ damage and are at greater risk of
stroke, MI, heart failure, and chronic kidney disease compared with patients
who have more easily controlled hypertension. Referral to a hypertension
specialist should be considered for in-depth evaluation and treatment.
Aldosterone antagonists are the most effective agents for lowering BP in
patients with resistant hypertension who are already on a three drug regimen.
Several device-based interventions, including renal denervation, carotid
baroreceptor activation, and an arteriovenous coupler device are under
investigation, but none of these technologies are currently approved for use in
the United States.
Lowering BP is but one mechanism by which cardiovascular risk can be reduced in hypertensive patients.
Irrespective of baseline cholesterol levels, statin therapy is recommended to
reduce the incidence of MI and stroke in patients at intermediate or high risk
of cardiovascular events. Low-dose aspirin also reduces cardiovascular event
rates in selected patients.








